Interview
How to end a pandemic in one jab
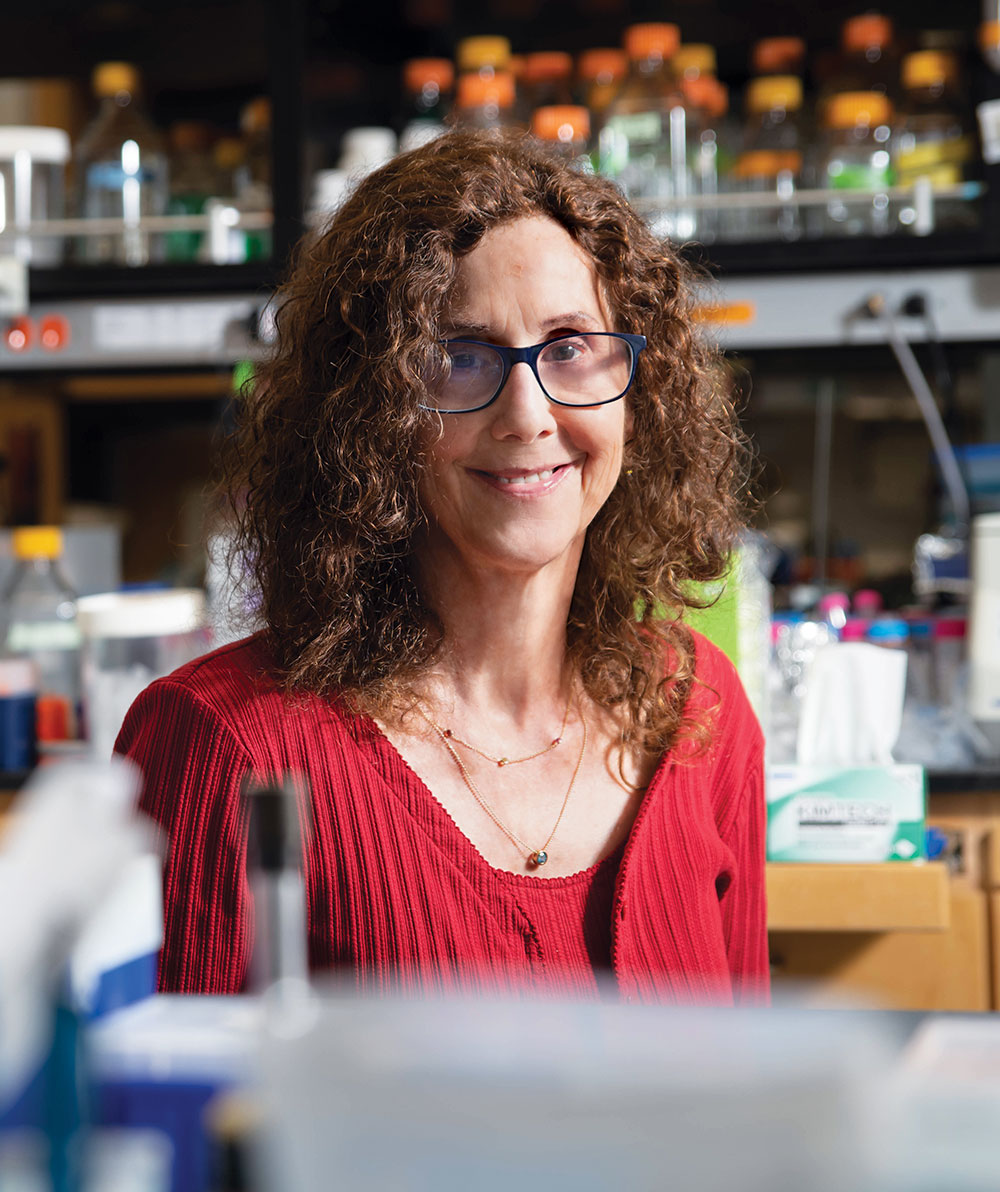
With Pamela J. Bjorkman
SARS-COV-2 is a wily shape-shifter. It mutates into new forms so frequently and expertly that even though scientists have reformulated vaccines in record time, we’ve already fallen behind. The arrival of a universal vaccine—one that could provide long-lasting protection against every variant—would signal a momentous turning point in the pandemic, letting us breathe easy despite the looming specter of even more virulent strains.
It’s not impossible. Universal vaccines for polio, measles, smallpox, and many other diseases offer protection for years or even a lifetime.
But it is extraordinarily difficult. Universal vaccines work by prompting the immune system to manufacture antibodies aimed at relatively fixed targets—the so-called conserved parts of a virus that rarely mutate. In the coronavirus, however, the conserved parts are largely sheltered inside the stems of its infamous spikes, while current vaccines aim at the spikes’ flashy tips. And although the tips are the most accessible parts of the virus, they are also the most frequently mutating—forming a halo of constantly moving targets. It’s a common problem; viruses like the ever-evolving influenza present vaccine makers with the same challenge. In fact, nearly a century of effort has failed to produce one universal flu shot.
Pamela J. Bjorkman isn’t daunted. A structural biologist at Caltech—and longtime collaborator of Rockefeller immunologist Michel C. Nussenzweig—she has spent decades studying how the immune system recognizes invading pathogens, working to develop therapeutics that make it respond in novel ways.
Bjorkman envisions a near future of universal vaccines for HIV, influenza, and the coronavirus. Though her efforts with HIV and influenza haven’t yet panned out, her work with SARS-CoV-2 may be about to hit the mark.
“Experts have been saying, ‘Wake up, world. This will happen again.’”
Recently, Bjorkman’s team reported in Science that they’ve created a new kind of training wheels for the immune system: a mosaic of different SARS-like coronavirus fragments arranged on nanoparticles. In animal models, the mosaic successfully sparked the immune system to produce antibodies against conserved parts of the coronaviruses and exhibited protection against both the original SARS-1 virus and the COVID-causing strain.
We spoke with Bjorkman about how this new approach might goose the immune system into seeing viruses differently.
With numerous therapeutics being developed against COVID, why is a vaccine still key to ending the pandemic?
I’ll give you a great example: Early in the pandemic, Michel Nussenzweig and his team isolated many different antibodies from infected people. Some were really potent. Companies then made drugs based on these types of antibodies, and they worked!
But of course, the virus mutated, and those antibodies don’t work as well anymore. Some, in fact, don’t work at all against newer SARS-CoV-2 variants like omicron, which has been able to evade even the most potent antibodies. We really need a pan-coronavirus vaccine that protects against everything that’s now out there and whatever might come next. But since coronaviruses differ so much, that might be extremely difficult or even impossible. So instead, my team is focusing on a coronavirus subset called sarbecoviruses, which have caused most of the recent spillover events—specifically, the original SARS-1 and SARS-CoV-2. We think a pan-sarbecovirus vaccine might be achievable.
Data
As of late last year, the WHO was monitoring 300+ omicron decendants.
How does your approach differ from that of current vaccines?
Most of the neutralizing antibodies we make against SARS-CoV-2, or in response to a vaccine, target the tip of the receptor binding domain (RBD) on the spike protein. That’s the region of the spike showing the most variability across SARS-CoV-2 variants and many sarbecoviruses. The RBD also has conserved parts—regions where the virus does not change often or at all. But these regions can be hard for antibodies to access, which could be partly why the immune system doesn’t naturally tend to make as many antibodies against them.
Our idea was to make a new target by gathering RBDs of eight different sarbecoviruses. And because the immune system tends to produce antibodies against identical pieces that are near each other, we randomly arranged 60 of these RBDs on each nanoparticle so that any two adjacent RBDs are rarely from the same virus. In a random arrangement, it’s the conserved parts of the RBDs, which are similar across sarbecoviruses, that are more likely to end up next to each other, making them more visible to the immune system. The goal is a vaccine that encourages the body to stop making so many antibodies against the variable RBD tip and instead make more against the conserved part of the RBD.
But you initially developed this approach for other diseases.
That’s right—we’ve spent five years making mosaic nanoparticles for influenza and HIV vaccines, but they didn’t work well in generating broadly cross-reactive antibody responses. To our immense surprise, the approach turned out to work quite well for sarbecoviruses, however. In animal models, we got the types of cross-reactive antibodies we wanted. And not only do they bind to and neutralize the different kinds of sarbecoviruses that were represented on the nanoparticles, these antibodies also target sarbecoviruses that weren’t represented in the mosaic. These mismatched neutralizing responses are very encouraging, because they show us what could happen in the event of a new viral spillover from animals to humans or when new SARS-CoV-2 variants emerge. It’s a strong suggestion that a future vaccine based on our approach wouldn’t need updating.
There’s always the question, however, of whether the virus will still be able to mutate its way into escaping from these cross-reactive antibodies. I don’t think that’s likely because of structural limitations inherent to the virus itself. But we are testing that possibility in collaboration with Rockefeller virologists Theodora Hatziioannou and Paul Bieniasz. Using a SARS-CoV-2 spike protein displayed on an engineered virus that can safely be grown in the lab, we’re looking for mutations that might occur after treatment with serums including antibodies derived from animals immunized by our mosaic.
You mentioned structural limitations in SARS-CoV-2. Are they the reason the mosaic strategy works well in this context?
The structural limitations are related to the position of the RBDs. The coronavirus’s spike can enter a host cell only when one or more of its RBDs assume an “up” position; that’s how it interacts with the cell’s receptor. But the spikes can go into a “down” position as well—specifically, to help evade immune responses. When the RBD is down, the conserved part meets the rest of the spike protein. We think when we target this region with antibodies, the virus cannot mutate in response—it must remain stable in order to assume the down position. Yet it hadn’t occurred to me when we started this work that this property of the RBD might be the whole key to why the mosaic approach seems to work for coronaviruses but not for other viruses.
Before COVID, some scientists kept research on coronaviruses alive even as public interest in them waned. Has the pandemic changed the calculus for how we support research into viruses that aren’t currently causing trouble but one day might?
I hope so, but I’m not sure. Every 10 years or so, we have one of these spillovers—first it was SARS-1, then MERS, and now SARS-CoV-2. And if you look through the coronavirus literature, experts had been saying for some time, “Wake up, world. This will happen again.”
But many researchers are already having trouble getting funding for coronaviruses. The same thing happened after the 2003 SARS-1 outbreak and after MERS as well. Once the storms passed, attention and support died down. Already with SARS-CoV-2, there are some who feel we’re done with this. They might say, “We have vaccines, and we can keep updating them and move on.” But I think that’s shortsighted.
In the United States alone, hundreds of people are still dying from the disease each day, and long COVID can be devastating (read more about the condition in “When COVID lingers”). SARS-CoV-2 variants continue to emerge, and there’s also the very real possibility that another animal coronavirus will spill over into humans; in fact, all that stands between us and a new pandemic is the emergence of a new virus that can infect humans and transmit asymptomatically. With respect to the current pandemic, it appears it could be making people more susceptible to other respiratory viruses, such as influenza and respiratory syncytial virus. So now we are seeing a worrying rise in cases for those viruses as well. I don’t see this as being over yet.