Interview
What if aging isn’t what we thought it was
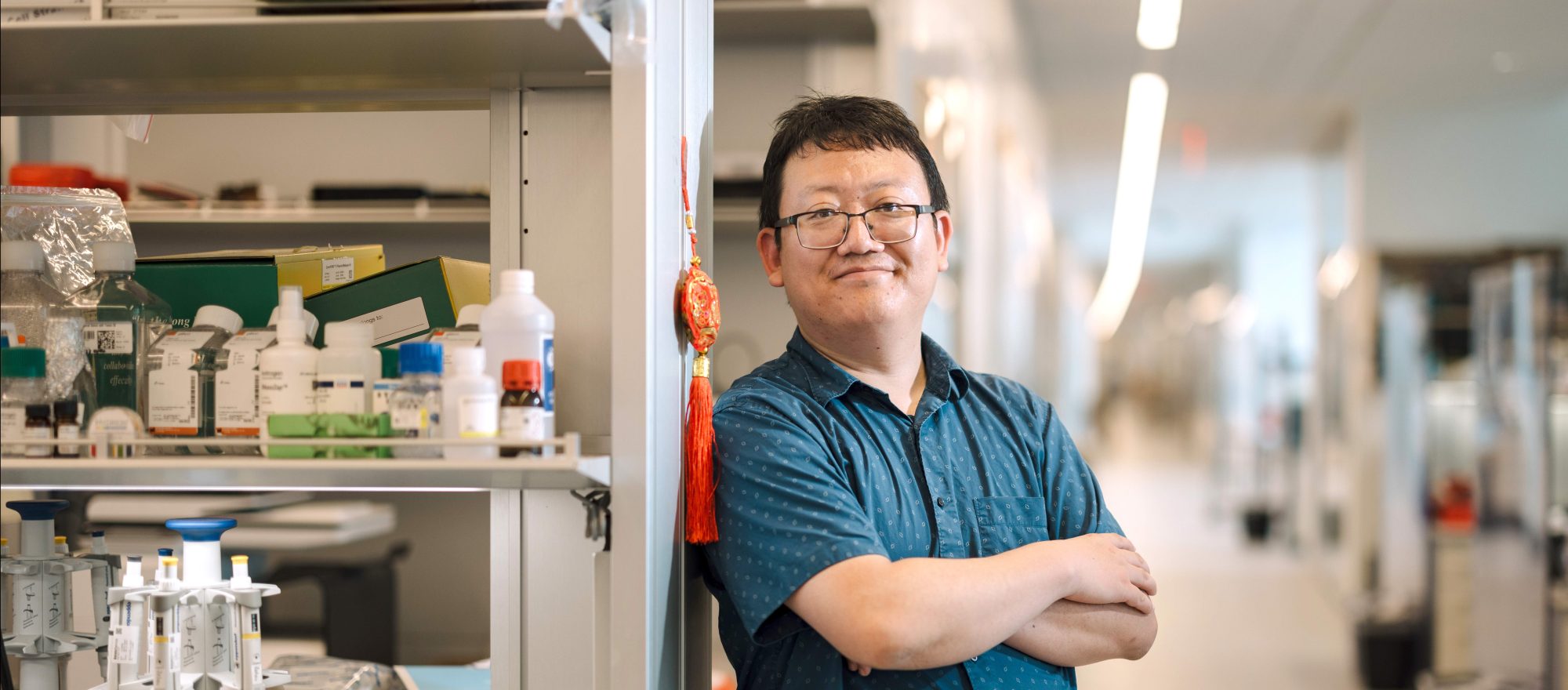
With Junyue Cao
What if aging weren’t just the result of years of wear and tear on the body, as is commonly believed? What if it were, as Junyue Cao has come to see it, another stage of development—one that could be regulated by thwarting age-related changes on the molecular level?
Should that become possible, it will be thanks largely to single-cell sequencing, a breakthrough technology that is transforming how scientists like Cao think about disease. When the technology came online in 2010, it offered researchers the ability to explore, for the first time, a handful of cells simultaneously. Each was a world unto itself, with its own dynamic ecosystem and distinct purpose in the body. The potential to explore the connection between cellular and biological health seemed infinite—as long as the technology could catch up with scientists’ ambitions for it.
As a Ph.D. student studying embryonic development at the University of Washington in 2015, Cao was perhaps one of the most ambitious. By then, single-cell sequencing could analyze several thousand cells at once. But Cao wanted millions. After all, the human body alone holds some 37 trillion cells, and not a single one is exempt from the effects of time. When he shared his goal with his colleagues, they gently told him that the idea was absurd.
Today, less than a decade later, he can sequence 20 million cells simultaneously—a remarkable advancement that has led him to intriguing new ideas about aging and disease.
As Rockefeller’s Fisher Center Foundation Assistant Professor and head of the Laboratory of Single-Cell Genomics and Population Dynamics, Cao uses his own tailored techniques—currently numbering eight—to study patterns of gene expression in single cells, illuminating how they differentiate into distinct types and maintain stability for as long as they can. In the process, he’s revealed various cellular mechanisms behind aging and disease, both of which involve the destabilization of cell populations.
Diseases, it’s now generally understood, don’t affect tissues uniformly; certain cell types deteriorate before others. If we could target these cells with anti-aging interventions at specific stages of life, he suggests, we might be able to transform the treatment of related conditions—and perhaps defy aging itself.
Data
Studies suggest adults tend to become happier as they age, reporting greater life satisfaction in their 80s than in their 20s.
How did your first major sequencing breakthrough come about?
In the first year and a half of my Ph.D., I tested about 200 different ways to increase the number of cells I could analyze at once, and nothing worked. I almost gave up. People kept questioning whether my goal was realistic, and I was getting nowhere.
But on New Year’s Day in 2017, I was in Florida with my family for the break, and I decided to analyze the data from my latest experiment on roundworm cells. I tested a bunch of enzymes to see which might be compatible with our platform. One called SuperScript IV had just become available. When I looked at the data, I was amazed. The enzyme was the key to making our technique work. I immediately emailed my Ph.D. mentor, Jay Shendure, and we were both so excited. For the first time, we had results as accurate as those produced by commercially available platforms, but we had the ability to profile many more cells.
Over the next year, I further improved the technique by testing hundreds of reactions. By the time I graduated, I was able to profile a million cells at a time.
What can your different methods now accomplish?
Among other things, we can track newborn cells throughout their lifetimes, identify thousands of new and rare cell types, pinpoint which cell numbers plummet during aging and which increase, and show how the same types of cells located in different organs behave in vastly different ways. Each technique is like opening a window that allows us to see unexpected things, and that lets us ask new questions.
When you joined Rockefeller, you switched to investigating the aging process. What have you learned in the last four years?
One thing we didn’t expect to discover is that, across cell types, there’s an enormous amount of variation in how they respond to aging and diseases such as Alzheimer’s. Some populations remain stable, but others drastically change, either in gene expression or in the size of the population. For example, we’ve seen that alterations in immune cells are really common, and that the changes differ from organ to organ. The immune system is almost certainly a key regulatory force in aging.
Each technique allows us to see unexpected things, and that lets us ask new questions.
So far, we’ve found more than 3,000 unique cellular states and 200 subtypes that undergo significant age-associated depletion or expansion. Within that, there is so much diversity between organs, ages, and sexes. For instance, female mice are more enriched with B-cell subtypes that are associated with autoimmune diseases, and that’s noteworthy because we know women have higher rates of autoimmune conditions.
Has your research made you rethink what’s happening to our bodies as they get older?
It has. Aging is generally seen as a steady accumulation of damage moving in a linear progression—the wear-and-tear theory. But our research implies that it’s more like a stage of development, where cell types greatly change in distinct time windows. For example, we’ve seen that some cell populations, such as stem cells in the brain and progenitor cells in muscles, are depleted in mouse middle age, which is about 40 in human years. But others expand in later stages of life. This correlates with some human studies that have found accelerated cell changes around age 40.
The idea of aging as a developmental stage seems like a new paradigm.
It is quite different from the current model, and yet it’s consistent with previous studies finding that successfully introducing anti-aging interventions is highly time-window specific. It may be that we need to intervene before critical cell types—stem cells or other progenitor cells, for example—disappear entirely.
There was a paper published in Science in 2022 that looked at whether the diabetes drug metformin—which has shown promise for treating various age-related ailments—could slow aging in mice at middle and very late stages. It turns out it’s effective only if administered during the middle stage.
We’ve also seen that there is some overlap of different types of cells changing in the same phase of life. Maybe they’re all regulated by a shared mechanism. If that’s true, perhaps we could target the mechanism itself.
If interventions are successful only at certain stages, does that mean ill-timed ones could have negative effects?
Potentially. For example, the population of inflammation cells just explodes later in life. So if someone receives a treatment that increases the proliferation of inflammatory aging cells, that could be harmful.
It’s also important to note that pinpointing which cell type changes occur at what stages can shorten the time needed to determine if a therapy works. If we know what types we’re targeting, we can quickly see if they aren’t being rescued in the target time window. That may also expedite identification of therapeutic targets. If some therapies are in the wrong time window, you could eliminate them right off the bat.
Is it possible that in the future, we’ll be able to dramatically alter how we age?
Thirty years ago, the idea that we could direct a cell to differentiate into almost any type desired would have sounded crazy. Now we can easily direct pluripotent cells to do just that. So if we do come to understand the cellular regulatory network—how different cells interact with each other during different stages to maintain the functions of the entire organism—in theory, we could engineer the human system to go beyond its current limitations.