
Feature
Taming the Threat
Vector-borne diseases are on the rise. But new treatments wait in the wings.
By Alexander GelfandMosquitoes, fleas, ticks, lice: Such humble creatures have played an outsized role in human history. During the Middle Ages, fleas carrying the bacterium that causes plague wiped out a third of Europe’s population. The Anopheles mosquito helped shape the course of the Revolutionary War, laying waste to British troops with its malarial payload. Overall, vector-borne diseases—those passed through living organisms acting as middlemen on behalf of germs and parasites—accounted for more illness and death from the 1600s to the early 1900s than all other causes combined.
As the 20th century progressed, however, the situation began to improve. In 1936, scientists at the Rockefeller Institute developed an effective vaccine against yellow fever, one of the world’s most dangerous mosquito-borne illnesses. Further advances in prevention, treatment, and vector control—including insecticides, drugs, and more vaccines—meant that by the 1960s, vector-borne diseases looked a lot more manageable.
And then something unsettling began to happen.
“The risk of catching a known vector-borne disease has been steadily going up. And new ones are surfacing all the time,” says Jean-Laurent Casanova, who has been investigating immune-system defects related to viruses spread by mosquitoes and ticks—aka arthropod-borne viruses, or “arboviruses.”
Indeed, relative newcomers such as West Nile virus and eastern equine encephalitis, and longstanding foes such as dengue and chikungunya, are all on the rise. (Instances of dengue alone have increased as much as tenfold since 2000, while West Nile is now the most common mosquito-borne illness in the United States.) Currently, these diseases kill more than 700,000 people annually, and leave many survivors with chronic disabilities.
Global travel, widespread deforestation, and rapid urban expansion are all partly to blame for this new reality. But a host of factors are at play. “Much has changed in recent years,” says James Logan, a medical entomologist at the London School of Hygiene & Tropical Medicine who runs the Global Vector Hub, an open-access resource for vector research and vector-control programs. “Climate change is driving the spread of vectors and the pathogens they transmit, without a doubt. Resistance to insecticides and drugs is also fueling the fire.”
Unfortunately, innovations in vaccines and treatments have not kept pace. At the heart of the problem lies a biological conundrum: Most vector-borne diseases are caused by viruses and parasites, which present extremely slippery targets. “Many of these pathogens have evolved to be super-variable to avoid being eliminated by the host immune system,” says Douglas Norris, an expert in vector and pathogen biology at Johns Hopkins University. As a result, until we can unpack the basic biology of these microscopic invaders—and our own immune responses to them—we have little hope of developing the necessary tools to ward them off.
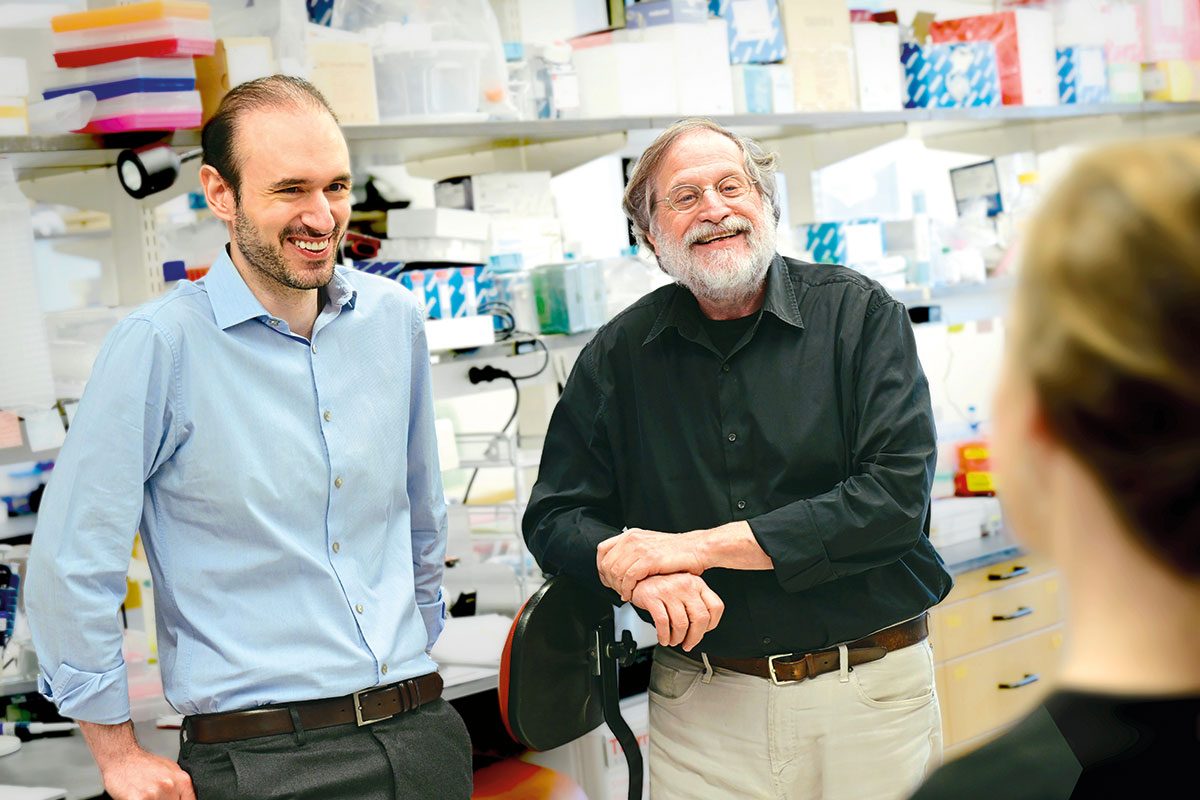
But Rockefeller scientists have long been studying these essential mechanisms. And many are leveraging the insights they’ve gained to inform novel ways of preventing and treating vector-borne diseases. Some, like Leslie Vosshall, concentrate on the organisms that spread these global threats. Others, like Charles M. Rice, focus on the pathogens that cause them. And still others, including Casanova, Jeffrey Ravetch, and Michel Nussenzweig, study the defenses our bodies mount against them, and how they sometimes go awry.
New discoveries in each of these areas will be crucial to tackling this large and growing list of diseases that, if left unchecked, could do even more harm in the future than they have in the past.
Wily adversaries

The very thing that gives vector-borne diseases their name—the organisms or “vectors” that spread them—also makes them particularly difficult to stamp out. For in addition to adding a layer of complexity to the chain of transmission, these tiny adversaries can be incredibly resourceful.
No one knows this better than Vosshall, head of the Laboratory of Neurogenetics and Behavior.
Vosshall began her career investigating olfaction in the fruit fly, as harmless an arthropod as one could encounter. But her fascination with how insects are led to their next meal by their sense of smell led her to Aedes aegypti, an elegant mosquito with white polka-dot markings that lives only a few weeks yet nonetheless manages to spread illnesses like dengue, Zika, yellow fever, and chikungunya with ruthless efficiency. Dengue alone menaces an estimated 4 billion people around the world, and while Aedes does not like the cold, that could soon prove much less of a deterrent. “As the globe warms, many more places in the United States and South America will become hospitable to these critters,” Vosshall says.
The Aedes aegypti mosquito lives only three weeks yet is nonetheless the most dangerous animal on earth. “As the globe warms, many more places in the United States and South America will become hospitable to these critters.” Vosshall
Vosshall uses genetic and behavioral experiments to examine everything from Aedes’ feeding behavior to its sex life. (Only female mosquitoes feed on blood, which they need to produce their eggs.) She’s revealing the animal’s basic biology in order to discover ways of rendering it harmless—for example, by interfering with its ability to perceive the cues it uses to hunt us, like the carbon dioxide we exhale and the heat we emit.
Numerous studies from Vosshall’s lab have repeatedly confirmed what a wily adversary Aedes is. More than a decade ago, she and her colleagues engineered a mutant version of the insect that could not sense carbon dioxide. It was, Vosshall says, one of the earliest efforts “to break the mosquito.” But while these mutants seemed innocuous when confined to the lab, they had no trouble locating human prey when released into more naturalistic environments. That finding was partially explained by a 2025 study, which revealed that mosquitoes became more sensitive to body heat after their olfactory sensors were knocked out, much as people develop more acute hearing after losing their sight. “These kinds of studies show that we’re dealing with a very, very formidable foe,” she says.
But that hasn’t stopped Vosshall and her team from dreaming up ever more creative ways of stymying Aedes.
Together with Laura Duvall, a former postdoc who is now on faculty at Columbia University, Vosshall identified a molecule called compound 18 that reduced Aedes’ appetite for blood. “It’s like Ozempic for mosquitoes,” Vosshall says.
When first discovered, large quantities of compound 18 were needed to kill a mosquito’s appetite, rendering it too costly for commercial use. But Vosshall and Duvall recently managed to increase the drug’s potency by a hundredfold, thereby also increasing the likelihood that a mosquito appetite suppressant might someday hit the market. Outdoor feeders filled with the compound could serve as mosquito snack bars, leaving the tiny bloodsuckers feeling too stuffed to pursue human beings.
Ph.D. student Jacopo Razzauti is taking a different tack, going back to the basics to improve one of the most effective tools we already have for deterring Aedes: insect repellents.
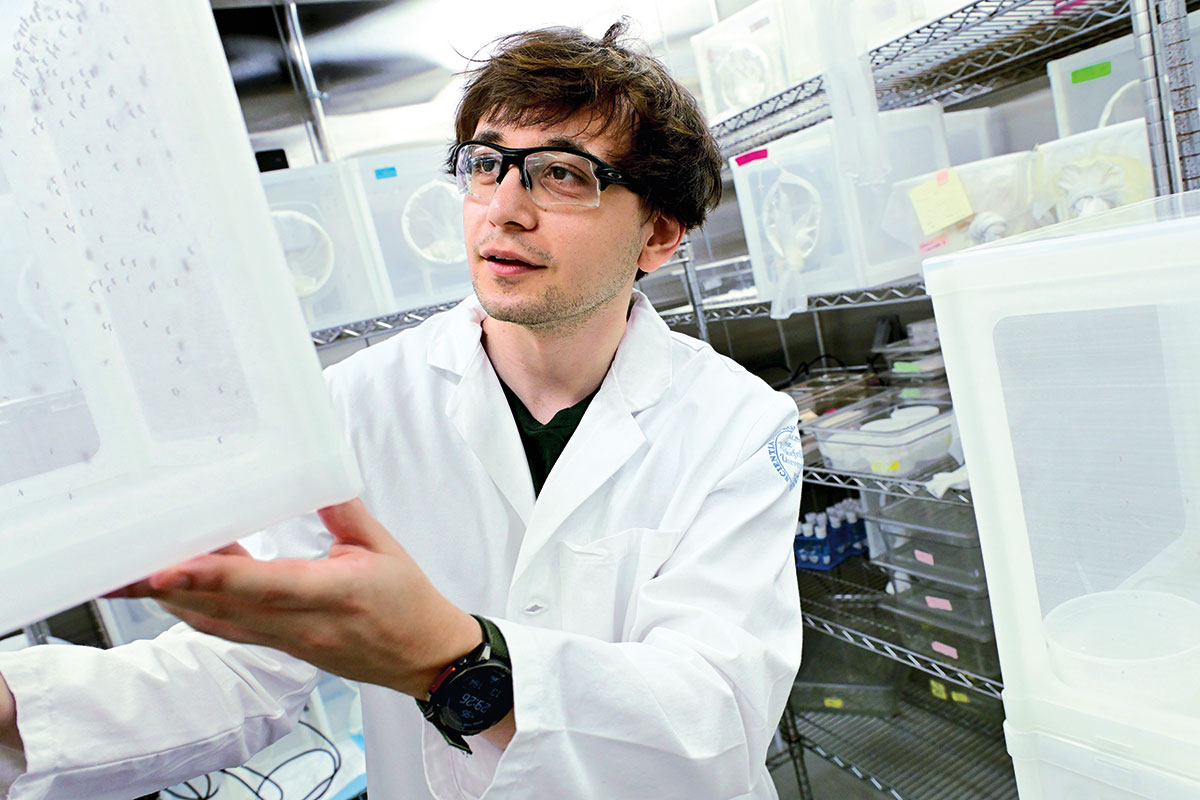
The two most popular, DEET and picaridin, have been around since the 1940s and 1980s, respectively. Yet we still don’t really understand how they work. And without knowing the precise mechanisms at play, scientists cannot rationally design better alternatives. (Neither repellent is 100 percent effective, and DEET, the gold standard, is stinky, greasy, and melts plastic.)
Razzauti is trying to solve the puzzle of repellency by capturing the precise moment when Aedes bounce off the invisible force field created by DEET and picaridin. Once that’s done, he plans to replicate the experience while imaging Aedes’ neuronal system.
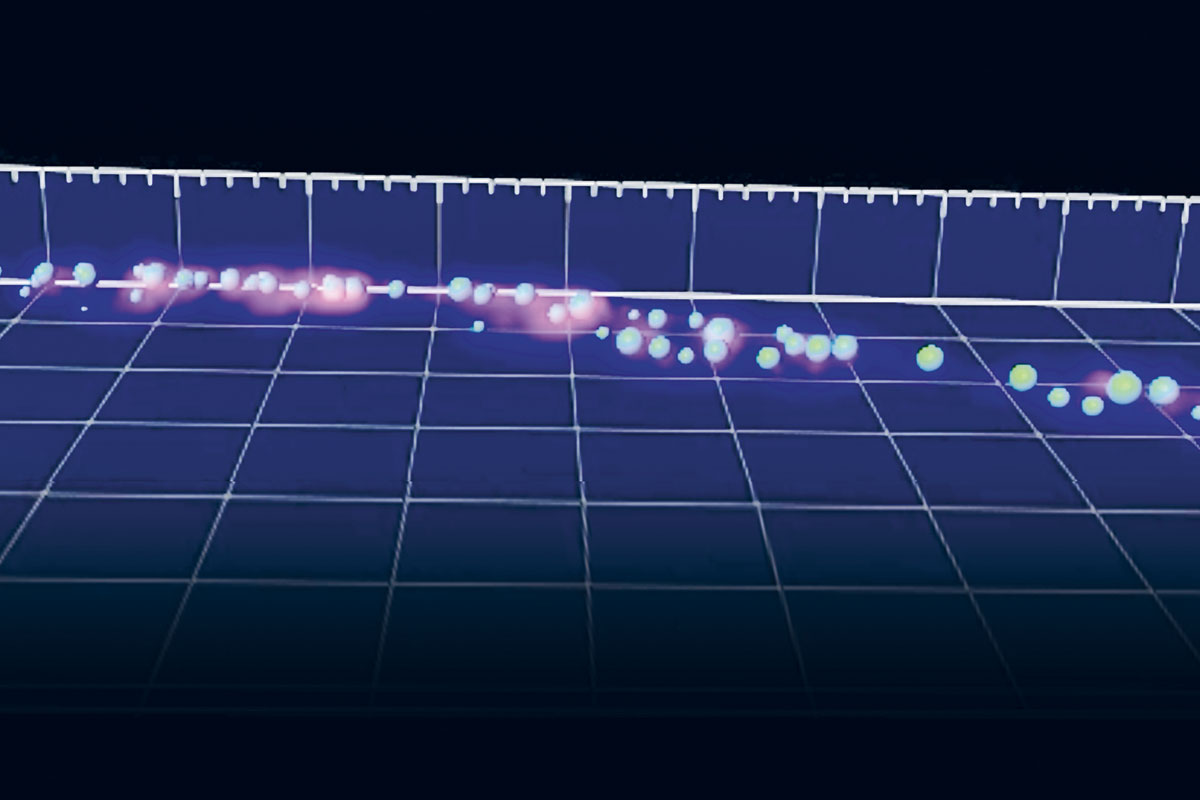
Razzauti has developed a machine learning algorithm that can track every single mosquito in HOSTel as it approaches and ultimately recoils from the repellents.
Razzauti has built a special chamber, dubbed the HOSTel, that can house multiple mosquitoes while administering all the things that make a host attractive: carbon dioxide, body odor, and heat. The chamber is equipped with a sliding door behind which Razzauti can position his bare arm—an enticing target for any female Aedes—protected by a bit of mesh. And because mosquitoes are too small and fast for the human eye to follow, it is also equipped with a high-speed camera that can record up to 500 frames per second. With help from data scientists at Rockefeller, Razzauti has developed a machine learning algorithm that can track every single mosquito in the HOSTel as it approaches and ultimately recoils from the repellents, capturing the precise instant when attraction turns to disgust.
Preliminary data suggest that the mosquito’s legs play an important role in sensing the repellents, so Razzauti has made custom-tailored cover slips that slide over Aedes’ delicate limbs like fingerless gloves. He plans to expose the tips of the animal’s legs to the repellents while imaging its neurons to determine exactly which cells respond and at what distance. Such data might finally answer the fundamental question of how repellents work, while also pointing the way toward more effective ones.
Inborn errors
Eighty percent of people infected with West Nile show no symptoms, and 19 percent experience mild ones like fever and joint pain. But 1 percent wind up in the hospital with encephalitis or meningitis—and 20 percent of those with encephalitis die.
West Nile is far from the only infection to provoke such wildly different outcomes; COVID, for instance, offered a stark illustration of another. Yet why and how such variability emerges has baffled doctors for decades.
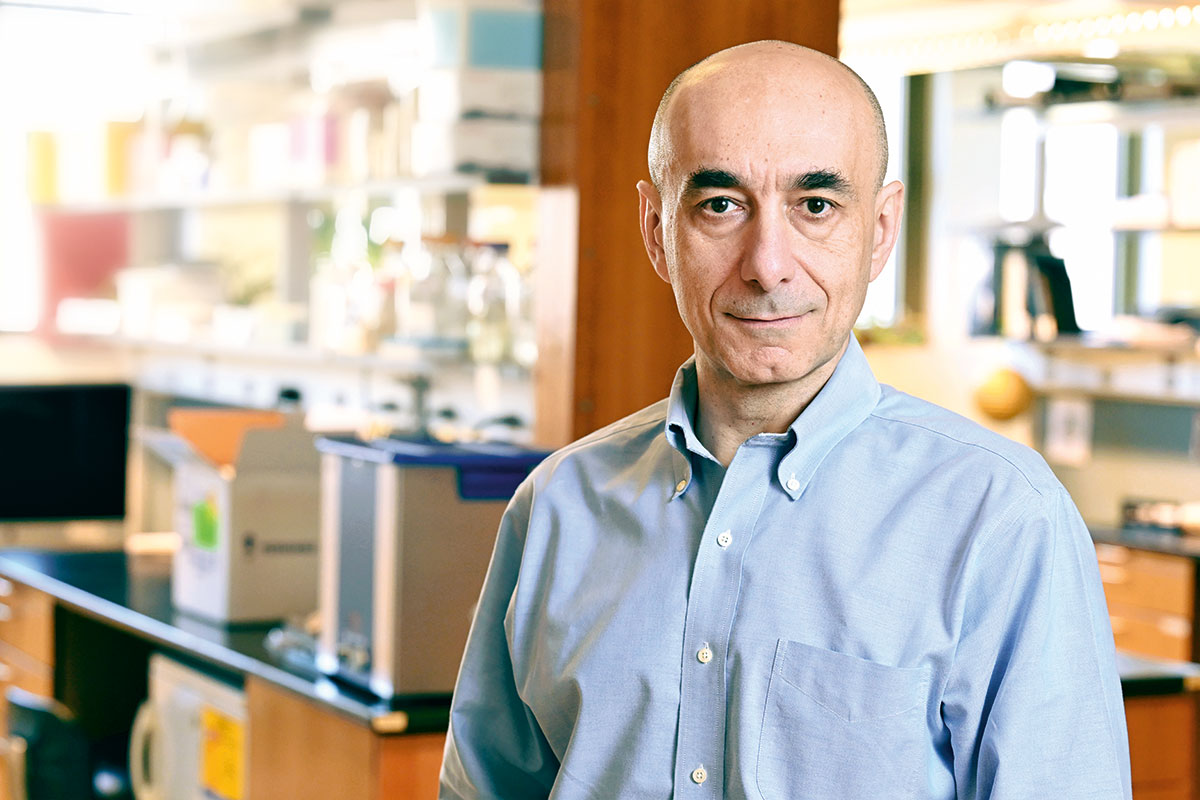
Casanova, head of the St. Giles Laboratory of Human Genetics of Infectious Diseases, has spent 30 years seeking answers to those questions. Since the 1990s, he has discovered hundreds of inborn errors of immunity, holes in our bodies’ defenses that make certain people particularly vulnerable to infection. He’s learned that some of these errors are genetic mutations that directly impair immune responses, while others manifest as autoantibodies that attack the very proteins we rely upon to repel viral and bacterial invaders.
In the depths of the pandemic, Casanova and his colleagues showed that 20 percent of COVID deaths were caused by autoantibodies that neutralize a group of immune system proteins called type I interferons. (He and others have found that the same autoantibodies cause 15 percent of critical MERS cases and 5 percent of critical flu cases.) Casanova estimates that up to 1 percent of people below the age of 65 produce such autoantibodies, a number that jumps to 5 percent after age 70, translating to 100 million people worldwide. And the older a person gets, the more potent the autoantibodies become. “Once the autoantibodies appear, it only gets worse,” he says.
Now Casanova has shown that these very same autoantibodies can have an even more significant impact on the severity of vector-borne diseases.
“A virus injected through a needle is not so different from one injected through the proboscis of a biting vector. “In essence, you could think of a mosquito or a tick as a kind of syringe.” Casanova
In 2019, Casanova and Rice, head of the Laboratory of Virology and Infectious Diseases, identified a genetic mutation that could provoke a life-threatening reaction to the yellow fever vaccine, a live vaccine that contains weakened yellow fever virus. Soon after, they demonstrated that a third of all such adverse reactions were caused by type I interferon autoantibodies.
Reasoning that a virus injected through a needle is not so different from one injected through the proboscis of a live animal—“in essence, you could think of a mosquito or a tick as a kind of syringe,” Casanova says—he wondered whether the same autoantibodies might cause severe disease in other arboviral infections.
Casanova first turned his attention to West Nile, which is spread by Culex mosquitoes that have in turn acquired it from birds. There is no vaccine or targeted antiviral treatment for the virus, and since arriving in the United States in 1999 (it was first isolated in Uganda in 1937), it has become the leading cause of mosquito-borne disease and epidemic encephalitis in the country.
In 2023, Casanova and an international team of collaborators published a study analyzing hundreds of patients hospitalized with West Nile in Italy, Hungary, and the U.S. Shockingly, they found that 35 percent of them—and a whopping 40 percent of patients with encephalitis—had type I interferon autoantibodies.
A follow-up study showed that the same autoantibodies cropped up in 10 percent of patients hospitalized with tick-borne encephalitis (TBE), an emerging health threat in Europe and Asia. Like West Nile, TBE also severely sickens a relatively small number of infected patients, but it leaves 10 to 20 percent of survivors with lasting neurological problems such as paralysis and cognitive impairment.
“It’s really devastating,” says Nussenzweig, who works on TBE with collaborators in Switzerland, where the disease is endemic.
A third study by the Casanova lab, published earlier this year, once again found high concentrations of type I interferon autoantibodies among severely ill patients infected with three emerging arboviruses: Powassan, a tick-borne illness found in North America; Ross River, which is spread by ticks in Australia and other parts of the South Pacific; and Usutu, which is transmitted by mosquitoes in parts of Europe, Africa, and the Middle East.
Casanova continues to work his way through the list of arboviruses, looking for the same autoimmune culprits. But he already thinks that elderly people should be routinely screened for them. Should they test positive, they can take steps to avoid both arboviruses and respiratory viruses and make sure to get any available vaccines—though not live ones.
Predictive biomarkers
If such wildly different outcomes weren’t perplexing enough, one mosquito-borne illness is associated with an even more curious phenomenon: People who contract dengue, a disease so painful that it’s known as “breakbone fever,” are at far higher risk of developing a life-threatening case specifically if they’ve had the virus before.
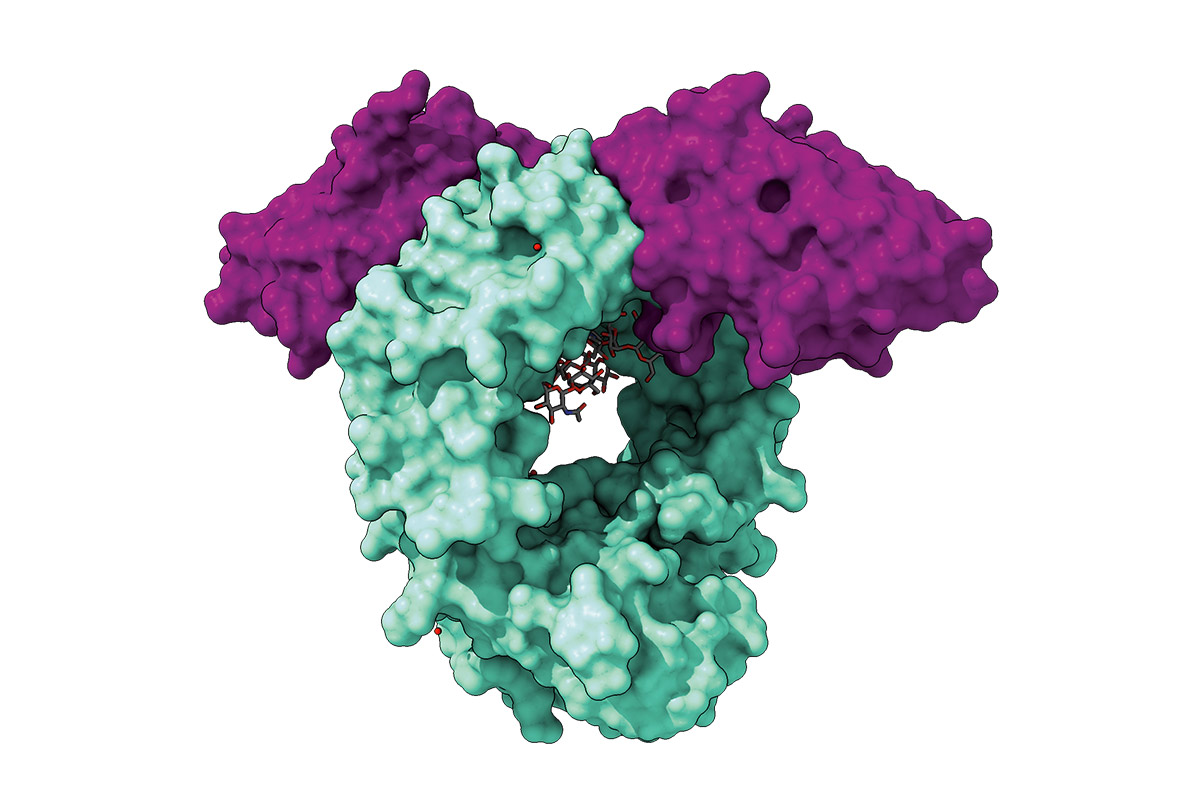
For many years, the prevailing theory was that leftover antibodies from prior infections somehow increased viral uptake, a phenomenon known as antibody-dependent enhancement, or ADE. But that never made much sense to Ravetch.
Ravetch, who heads the Leonard Wagner Laboratory of Molecular Genetics and Immunology, knew that people with mild and severe disease had the same levels of virus in their blood. He had other reasons for suspecting that something else might be going on: For decades, Ravetch has studied a structural component of antibodies known as the Fc region that can both promote and inhibit inflammation. Over time, he has shown that subtle molecular changes to the Fc and its corresponding receptors can turn otherwise protective antibodies pathogenic and vice versa. Ravetch therefore wondered if such modifications might underlie ADE, which can lead to deadly conditions such as hemorrhagic fever and septic shock.
The first evidence this might be true came in 2017, when Ravetch and his colleagues discovered that patients with severe dengue had antibodies whose Fc lacked a particular sugar, a chemical alteration known as afucosylation. In a subsequent study conducted with the help of researchers at the Pasteur Institute in Cambodia, the Ravetch lab demonstrated that afucosylated antibodies could serve as a predictive biomarker for people at risk of developing severe disease, a finding that could allow clinicians in the developing countries where dengue is most common to concentrate their resources on the highest-risk patients.
“In settings like field hospitals in resource-limited countries, this is a big deal,” says Stylianos Bournazos, a research associate professor in the Ravetch lab who led the Cambodian study.
The Ravetch lab showed that certain antibodies could serve as a predictive biomarker for people at risk of developing severe disease. “In settings like field hospitals in resource-limited countries, this is a big thing,” says Bournazos.
Testing people for afucosylated antibodies, however, is a slow and expensive process. So the lab developed a synthetic antibody, known as a nanobody, that could be used to screen for afucosylation quickly and cheaply. As a bonus, in 2023, Ravetch and his colleagues showed that the same nanobody could also block the activity of afucosylated antibodies in mice, raising the possibility of a dual-purpose tool that could serve not only as a rapid diagnostic for severe dengue, but also as a treatment. With help from the Rice lab, Ravetch also developed a mouse model that allowed him to trace the specific mechanism whereby afucosylated antibodies cause life-threatening complications.
More recently, the Ravetch lab teamed up with collaborators at Emory University to isolate an enzyme that can also prevent severe dengue in mice, suggesting another potential treatment—one that shows promise for a variety of other inflammatory and autoimmune conditions as well. And Ravetch is currently collaborating with Casanova to see if afucosylation might drive other instances of severe arboviral disease, and to explore the possible interplay between Fc modifications and type I interferon autoantibodies.
Bournazos, meanwhile, is taking a deep dive into a different arbovirus: chikungunya, which has spread to more than 60 countries on the wings of Aedes aegypti. Unlike dengue, chikungunya causes symptoms in nearly everyone who contracts it, and in almost 50 percent of patients, some of those symptoms, such as disabling joint pain, can persist for months or even years.
Again, with assistance from the Rice lab and his Cambodian collaborators, Bournazos aims to learn whether an abnormal antibody response is to blame for chronic chikungunya, and, if so, whether changes to the Fc can once again serve as a predictive biomarker. In this case, however, the goal would be to improve care by identifying—and perhaps, someday, even treating—patients at risk of chronic, rather than severe vector-borne disease.
Enhancing defenses
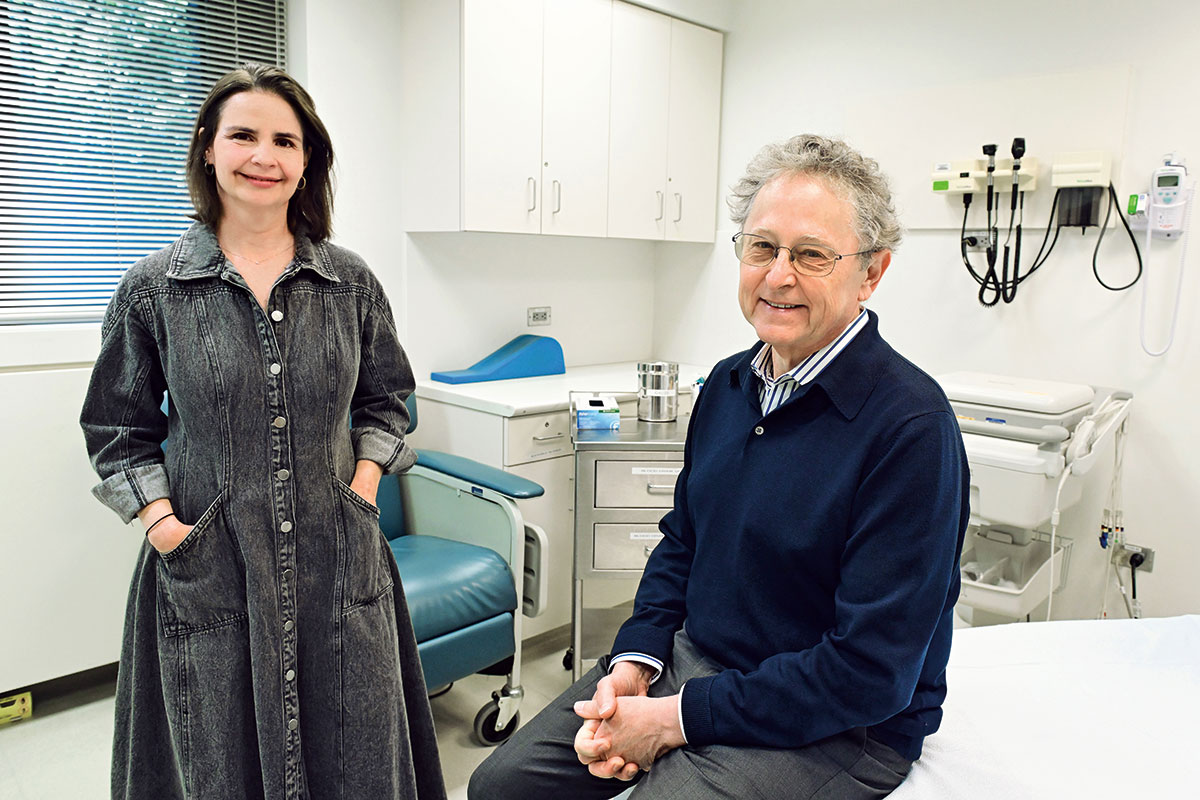
If Ravetch and Casanova are interested in those cases where the immune system fails to defend against vector-borne diseases, Nussenzweig is interested in the ones where it succeeds.
Nussenzweig has spent decades studying antibodies and the immune cells that produce them. Along the way, he has established a track record of finding and enhancing highly potent human antibodies to treat and prevent viral diseases. He and his close collaborator Marina Caskey, a professor of clinical investigation, honed this approach to antibody therapy against HIV and have since applied it to SARS-CoV-2 and hepatitis B. The duo first turned their attention to vector-borne diseases during the 2015-2016 Zika epidemic, which had its epicenter in Brazil—the same country where both happen to have been born.
As with dengue, most Zika infections are mild or asymptomatic. When the virus infects pregnant women, however, it can have catastrophic consequences for their babies. During the Brazil outbreak, thousands of children born to infected mothers developed microcephaly and other serious neurological problems.
“Zika was a terrible tragedy for Brazil, so we were both interested in seeing if we could learn something about human immunity to the virus—and find some potent antibodies that would be protective against infection,” Nussenzweig says.
“Zika was a terrible tragedy for Brazil, so we were both interested in seeing if we could learn something about human immunity to the virus—and find some potent antibodies that would be protective against infection.”Nussenzweig
Together with Davide Robbiani, a former lab member who now directs the Institute for Research in Biomedicine in Switzerland, Nussenzweig and Caskey isolated potent anti-Zika antibodies from the blood of infected patients. By modifying the Fc of the most effective one, they managed to increase its half-life to the point where it could potentially protect a pregnant woman’s embryo throughout the period when the virus is most likely to do serious damage.
The Butantan Institute, a state-run biomedical research institution in Brazil, is currently gearing up to produce this engineered antibody for clinical use in hopes of preventing infection in women who are pregnant or wish to be. “You could offer it to people that are about to be or are already pregnant to bridge them safely through the pregnancy,” Caskey says.
Now the team is looking to repeat that success with another vector-borne disease that can have devastating effects: TBE.
There are several effective vaccines against TBE. But uptake has been low for reasons including cost, access, and vaccine hesitancy, and there are no targeted therapies for people who contract the illness. As a result, while severe cases remain relatively rare, “it’s a bad disease without any options,” Nussenzweig says.
That may soon change. With support from the Stavros Niarchos Foundation Institute for Global Infectious Disease Research, Nussenzweig, Caskey, and Robbiani have developed a potent antibody against the TBE virus. They have already demonstrated that the antibody can treat and prevent TBE in mice and plan to begin testing it in Swiss volunteers this fall. (Two other Swiss research groups are also involved, as is the Swiss National Reference Center for tick-borne diseases, which will help recruit participants.)
As with the work being done by his colleagues in labs across campus, Nussenzweig’s research could have broader implications. For example, the anti-TBE antibodies that he identified showed activity against other tick-borne viruses, including Powassan, which can also leave survivors with lasting neurological problems. And Nussenzweig is looking into possible collaborations with researchers in Australia, home to a variety of arboviruses, on other vector-borne diseases.
A united front
The pace at which these scientists are producing new ways of managing vectors and the diseases they transmit may seem astonishing. After all, each has turned out studies in the past few years that could revolutionize the way we treat and prevent everything from West Nile virus to TBE and beyond.
Yet all these successes were built on decades of painstaking research. Vosshall’s work on Aedes aegypti grew out of an insatiable curiosity about the mechanisms underlying olfaction in insects and humans. Casanova’s work on arboviruses sprang from his larger quest to understand why some people become deathly ill from infections while most do not. Ravetch’s work on dengue and now chikungunya emerged from his desire to understand how antibodies can have both destructive and protective effects. And Nussenzweig came to antibody therapy through his fascination with the fundamental building blocks of the immune system.
All hoped that their research would help improve health and alleviate suffering. But none could have envisioned exactly where it might lead. Such is the power of practicing science even when the practical benefits may be decades away—and all but impossible to predict in precise detail.
“It does come full circle,” says Ravetch. “But it takes a lot of long-term thinking.”