Feature
Clinical Trials
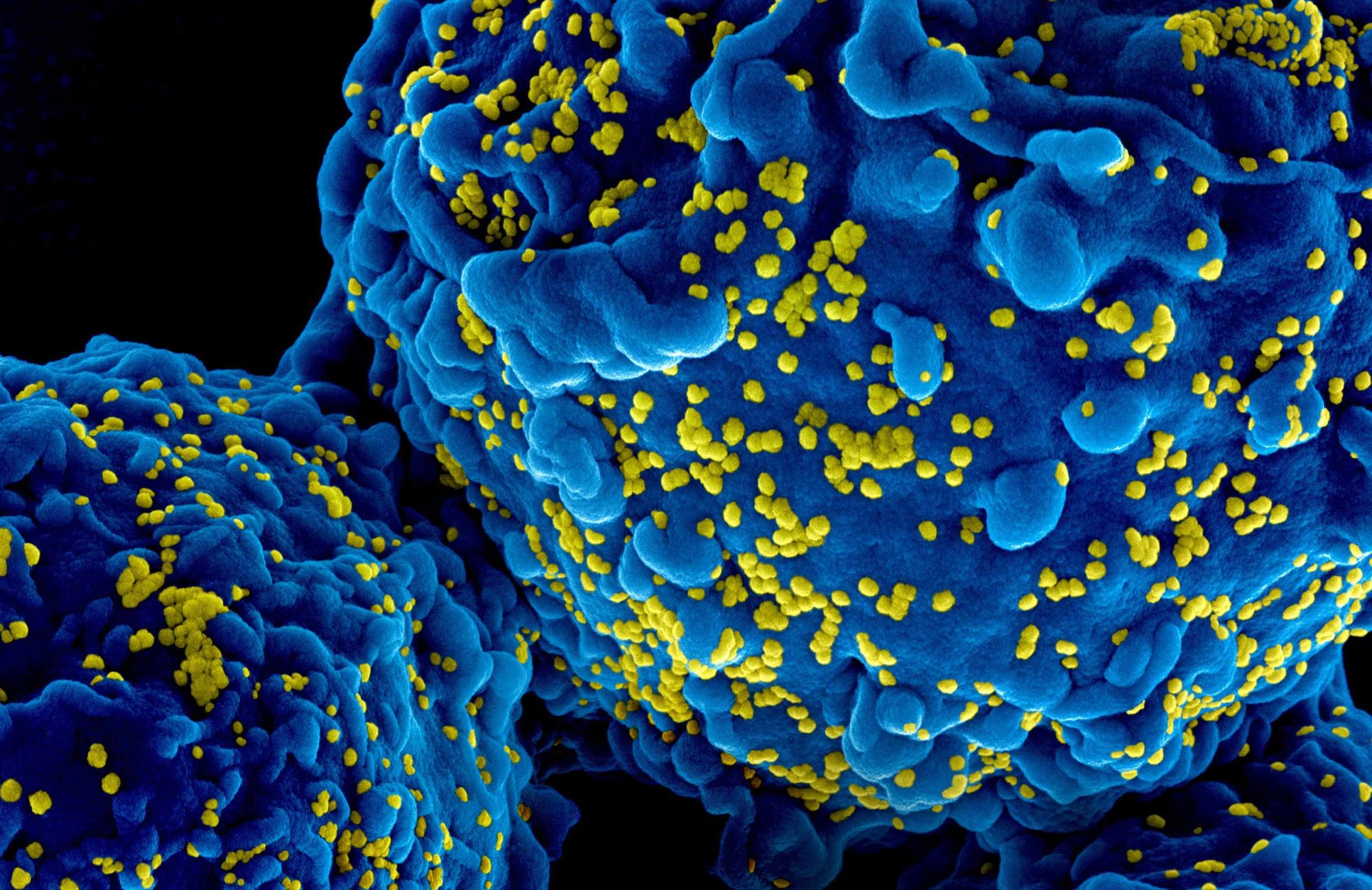
By Sarah C.P. WilliamsThe beginning of the end of HIV?
New antiretroviral treatment puts HIV remission on the table—and the possibility of an eventual cure more likely.
For decades, treating HIV has meant a daily battle against a virus that never truly leaves the body. Antiretroviral drugs can suppress HIV to undetectable levels, but a missed dose or loss of access to care can make the virus come roaring back.
But recent clinical trial results are finding something extraordinary: an HIV treatment that could keep the virus at bay for six months with a single injection.


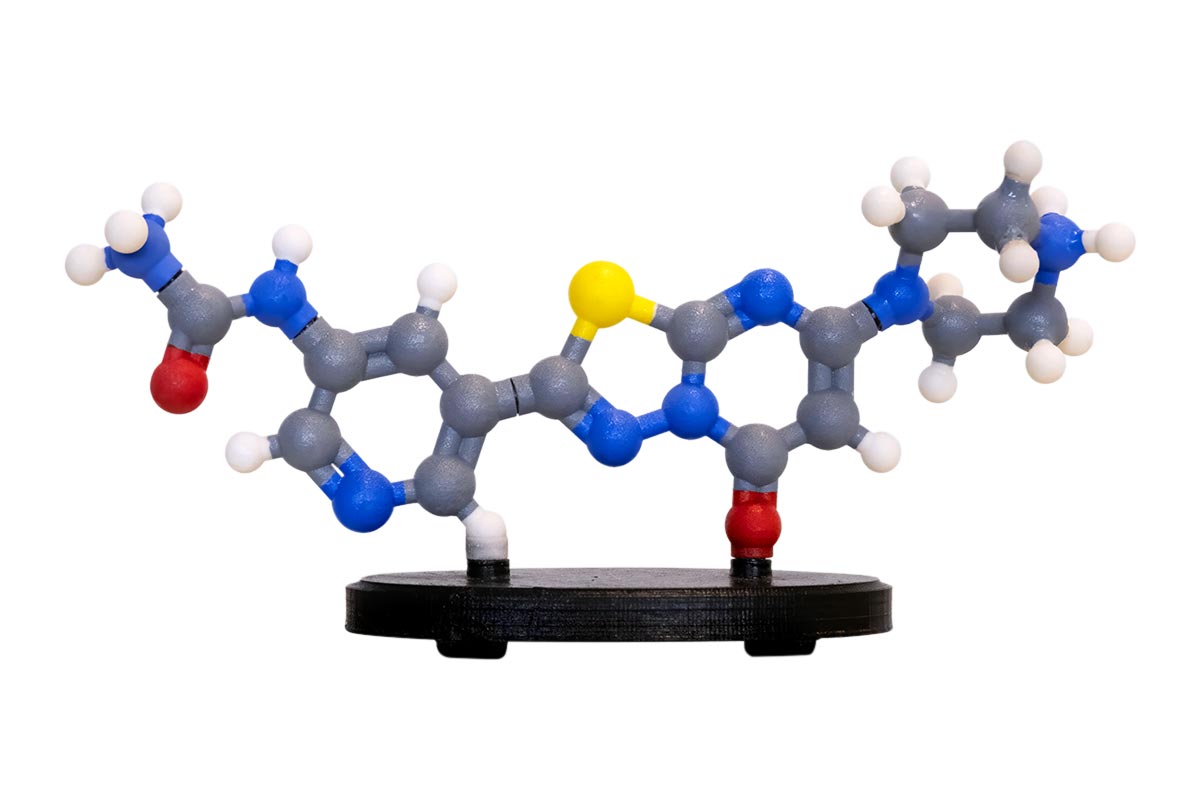
At the heart of this research are broadly neutralizing antibodies (bNAbs), proteins that bind to HIV, blocking infection and enhancing the immune system’s attack on the virus. Unlike typical antibodies, bNAbs can target many different HIV strains, making them especially valuable against the rapidly mutating virus.
The antibodies were first discovered, and fine-tuned for clinical use, in the lab of Michel C. Nussenzweig and Marina Caskey. Now, biopharmaceutical company Gilead Sciences—which has licensed the antibodies from Rockefeller—is carrying out Phase 2 trials, testing their safety and efficacy in patients with HIV.
In March, Gilead presented data showing that a combination of bNAbs—along with the long-acting antiretroviral drug lenacapavir—given every six months led to undetectable levels of virus in 96 percent of study participants, numbers comparable to standard daily treatment regimens.
“Seeing that data from Gilead was incredibly exciting and reassuring,” says Nussenzweig, the Zanvil A. Cohn and Ralph M. Steinman Professor and an investigator at the Howard Hughes Medical Institute. “This is what we thought would happen, but having it validated is just amazing.”
Nussenzweig first identified the antibodies, known as 3BNC117 and 10-1074, while studying “elite controllers”—individuals living with HIV whose immune systems have a powerful ability to neutralize the virus, preventing them from developing symptoms of disease.
Isolating and studying the antibodies was only possible because of a method Nussenzweig pioneered in 2009 to find immune cells that make desired antibodies and manufacture those cells in the lab. He and Caskey have used the same approach to develop antibodies against diseases, including malaria, Zika, and COVID-19. Now, they are also using it to tackle hepatitis B.
In the case of HIV, bNAbs work by recognizing and binding to specific proteins on the surface of the virus that are essential for it to infect cells. The antibodies directly block HIV from infecting cells and also recruit the immune system to find and destroy already-infected cells.
“These two antibodies showed really strong activity against the virus and had a number of other qualities that told us they might work in patients,” says Caskey, a professor of clinical investigation.
“To be able to switch patients from daily pills, or injections every two months, to a treatment just twice a year would be a huge advance to the field.”
Early trials led by Nussenzweig and Caskey showed that single infusions of the antibodies sharply reduced viral levels, and combining them made the effects even longer lasting. Moreover, giving multiple treatments together makes it harder for the virus to mutate resistance.
In 2020, Gilead licensed long-acting versions of 3BNC117 (now teropavimab) and 10-1074 (now zinlirvimab) from Rockefeller, which retained rights for early-stage research aimed at improving the antibodies’ effectiveness.
Since then, the work has progressed into a promising new phase. In 2023, Gilead’s Phase 1b trial showed that combining teropavimab, zinlirvimab, and the long-acting drug lenacapavir suppressed the virus in 90 percent of participants for six months. The more recent Phase 2 results, on a larger patient population, showed even more encouraging data. Those results came on the heels of a January decision by the FDA to grant the drug combination Breakthrough Therapy designation, which is given to treatments that show early promise of being significantly more effective than existing options.
“To be able to switch patients from daily pills, or injections every two months, to a treatment just twice a year would be a huge advance to the field,” says Caskey. “For a significant number of people with HIV, it’s challenging to take daily medication.”
Although Gilead is focusing on refining these antibodies as a viable treatment, Nussenzweig and Caskey are still pursuing broader questions through exploratory research funded by the Stavros Niarchos Foundation Institute for Global Infectious Disease Research, the Gates Foundation, and the National Institutes of Health. Their goal is to use bNAbs to achieve remission—control of HIV without ongoing therapy.
“The exciting thing in this field right now is that we have a much better understanding than ever before of what holds people back from being cured.”
Caskey’s recent studies suggest that when the antibodies are given at the same time as standard HIV drugs, they seem to boost certain immune cells that are particularly good at recognizing and attacking the virus. In a few cases, this improved immune response has allowed individuals to maintain undetectable or very low levels of the virus for years without daily medication. Caskey is also investigating whether the antibodies can target “hidden reservoirs” of HIV that allow the virus to rebound when treatment stops.
“The exciting thing in this field right now is that we have a much better understanding than ever before of what holds people back from being cured,” says Nussenzweig. “The basic science progress over the last five years has been huge, and we now have an inkling of how to change the course of disease in a rational way.”
The latest results out of Gilead, he says, may be just the beginning of how bNAbs could revolutionize the treatment of HIV.
A faster clot-buster for heart attacks
Zalunfiban, a cutting-edge injectable that inhibits platelet clumping, represents the culimination of decades of life-saving research.
Picture this: A man in his 60s is mowing his lawn when a sudden, crushing pain rips through his chest. His arm feels heavy, his breathing labored. Panicked, his wife calls 911.
Within minutes, paramedics arrive and realize the man is having a heart attack; a clot in a major artery is blocking the flow of blood to his heart. Immediately, they pull out a small injector containing zalunfiban—an experimental new medication developed by Barry S. Coller, who heads the Allen and Frances Adler Laboratory of Blood and Vascular Biology and is the physician-in-chief at the Rockefeller University Hospital. Unlike heart attack treatments that require injection directly into a vein, zalunfiban can be injected just under the skin, like an at-home insulin shot or EpiPen.

Within 15 minutes, the drug has stopped blood platelets from clumping together, preventing the formation of additional clots and giving the blocked artery a chance to reopen. Because it acts so fast, the medication buys him time, keeping blood flowing through the heart rather than letting tissue become permanently damaged en route to the hospital.
For years, doctors have performed life-saving procedures to open closed arteries once patients arrive at the hospital. But the real danger often happens before they get there. Half of all heart attack deaths occur before a patient reaches the emergency room; the further someone lives from a hospital, the worse they tend to fare. Zalunfiban, currently in Phase 3 clinical trials running on two continents, aims to change that.
“We hope that zalunfiban will save lives,” says Coller, who is also The David Rockefeller Professor and vice president for medical affairs. “If successful, it could eventually be in every ambulance, and someday, even in medicine chests of people at high risk of having a heart attack.”
Coller has spent more than five decades studying how platelets clump to form clots—a process essential to stop bleeding but dangerous when it occurs in the heart or brain. His first breakthrough came with abciximab, an antibody targeting the platelet receptor that binds fibrinogen, a protein that supports clumping by bridging between platelets.
Abciximab was approved by the FDA in 1994 and given to millions of patients undergoing artery-opening procedures. But it had one big drawback: It had to be given intraveniously through an IV controlled by an electric pump, limiting its use primarily to hospitalized patients.
“With abciximab, it became really clear that the people who were treated earlier were the ones who got the greatest benefit,” says Coller. “So the question for me became: How do we get a drug that potently and predictably inhibits platelet clumping to patients even earlier?”
In 2001, Coller joined Rockefeller, where he worked with the university’s cutting-edge drug screening facility to search for chemical compounds—small molecules instead of antibodies—that could block the interaction between platelets and fibrinogen. The first hit was dubbed Rockefeller University Compound 1, or RUC-1. With colleagues at the Mount Sinai Icahn School of Medicine and the National Institutes of Health, Coller refined that molecule so that it locked platelet receptors into an inactive state, leading to RUC-2 and ultimately RUC-4.
RUC-4 acts within minutes after injection, eliminating the need for controlled intravenous delivery. Importantly, its effect wears off in about two hours—which complements treatments that take longer to take effect and diminishes the risk of excess bleeding if surgery needs to be performed.
“We hope that zalunfiban will save lives. If successful, it could eventually be in every ambulance, and someday, even in medicine chests of people at high risk of having a heart attack.”
In 2017, Rockefeller licensed RUC-4 to CeleCor Therapeutics. Coller became its chief scientific advisor, continuing to advance RUC-4 (now zalunfiban). Initial testing in healthy volunteers and patients on daily aspirin went well, leading to a small Phase 2 trial in the Netherlands. There, 27 patients treated in the hospital for heart attacks were given varying doses of zalunfiban to test its effect on their arteries in just the brief time period in which they were being prepared for artery-opening procedures.
“This study was not designed to directly assess whether zalunfiban opens arteries, but it was gratifying to see that the higher doses were associated with a strikingly higher percentage of open arteries with good blood flow,” Coller says.
In 2021, CeleCor began a Phase 2b trial to study zalunfiban in ambulances—finally using the drug as an early intervention, exactly what Coller had been aiming for when he set out to develop it almost 20 years before. After consulting with the FDA, CeleCor converted the trial to a Phase 3 trial aiming to assess the drug’s safety and efficacy.
Today, that trial is ongoing at dozens of hospital systems in Europe, Canada, the U.S., and Mexico. In some locations, prefilled syringes of zalunfiban are stored in ambulances associated with these hospitals, ready to be injected into patients as soon as a heart attack is suspected. At others, zalunfiban is administered as soon as a patient arrives. Data on the patients—so far, more than 2,350 of them—is being collected for one year after their treatment. CeleCor is aiming to present and publish the first results in late 2025.
The hard work to reach this moment has been well worth it, Coller says: “I saw that there were people dying who I thought didn’t need to die. I had to try to help.”