
Interview
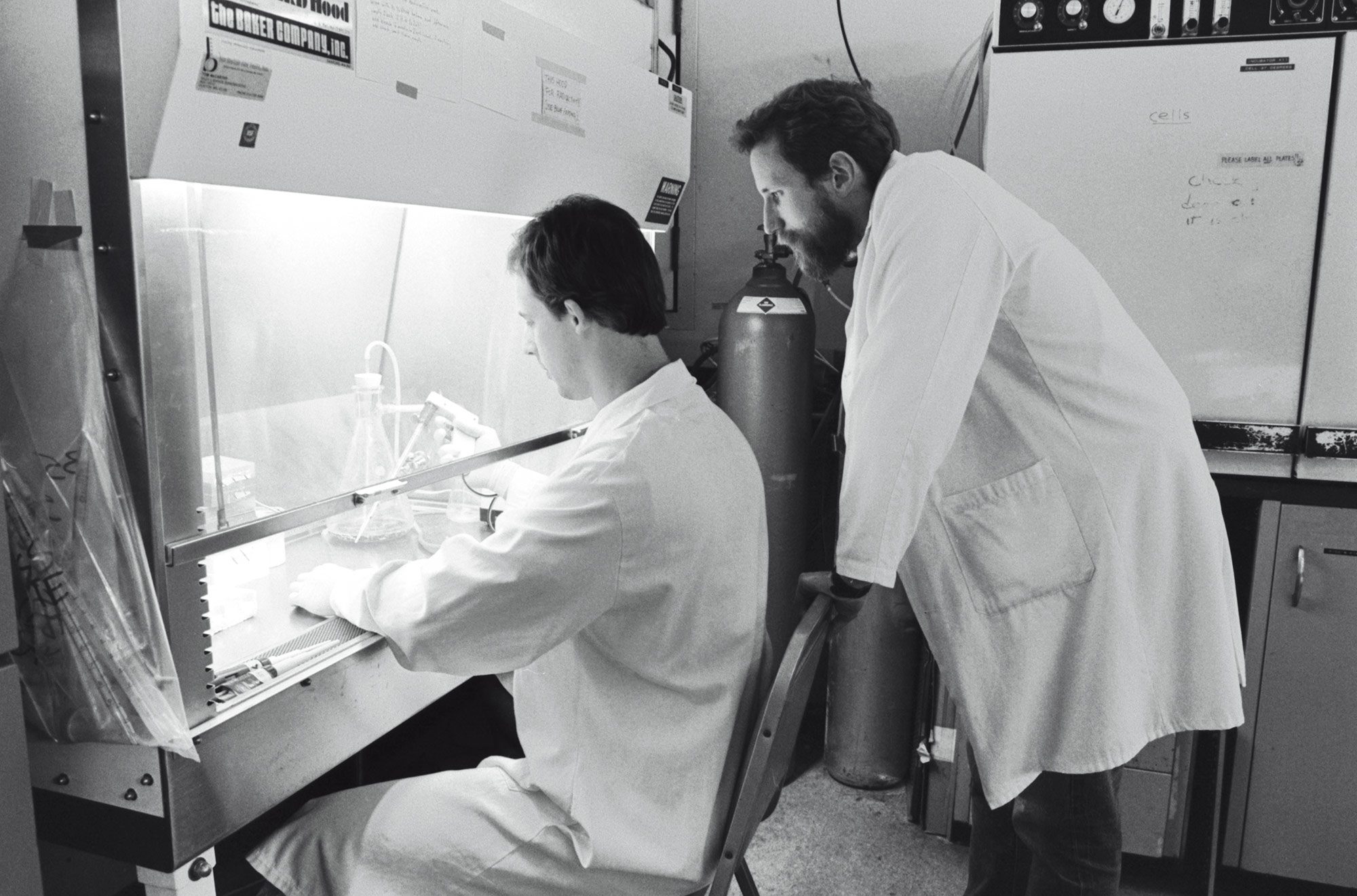
Charles M. Rice
When experiments keep failing, is there a time to call it quits? Meet the scientist who spent decades of his life chasing after hepatitis C before his efforts helped produce a cure.
By Jessica Wapnercharlie rice first began work on the hepatitis C virus in 1989, when it seemed like a straightforward project. The hope was that a vaccine could be modeled after one that had successfully eradicated yellow fever from much of the world.
But the virus proved inscrutable. The vaccine never materialized, and it took decades of study before an effective treatment could be created—a combination of antiviral drugs that became available in 2013 and are credited with saving hundreds of thousands of lives.
For his pivotal role in the development of this therapy, Rice, Maurice R. and Corinne P. Greenberg Professor in Virology, was awarded the Lasker-DeBakey Clinical Medical Research Award last fall alongside two other scientists. We spoke with him about the highs and lows of his 30-year quest to cajole the virus into a form scientists could work with.
When you first began researching the hepatitis C virus, did you know what a vexing foe it would prove to be?
Yes and no. Certainly the mystery of identifying the virus in the first place hinted at the complicated future to come. For many years, we knew that there existed some entity in blood that was neither hepatitis A nor hepatitis B. But until that entity was found, we could only refer to it as non-A, non-B hepatitis. That cumbersome name really foreshadows how hard this virus would be to pin down.
Yet there were reasons to think we could readily stop the virus in those early years, too. When the hepatitis C virus (HCV) was finally identified, in 1989, scientists saw that it was a member of the same family as the virus that causes yellow fever. The yellow fever vaccine is one of the safest and most effective immunizations available, so it was easy to imagine that creating a vaccine for HCV would not be too arduous.
In fact, back in the late 1980s, when I was at the Washington University in St. Louis, my lab was working on a molecular clone of the strain of the yellow fever virus that was used in the vaccine, and my group, in concert with others, tried to use that clone to create an HCV vaccine. It seemed like a logical approach, considering the similarity between these two pathogens.
So what happened?
As it turned out, the features that distinguish HCV from yellow fever and other viruses also make it a challenging target for a vaccine. More than 20 years later, we are still waiting for an HCV vaccine.
When did you turn your attention to searching for a cure?
We realized that if we wanted any chance at finding a treatment for HCV, we needed to be able to study it outside of people—in cell cultures and animal models. But when we tried to coax the virus to replicate in cells in the lab or in animals, it mostly didn’t work. We used all the classic techniques, which used the genome of the virus to initiate replication, but failed.
Eventually we started to wonder: Were we actually working with the correct genome sequence for the virus? RNA viruses like HCV won’t replicate if a portion of the genetic sequence is missing. And indeed, when we reevaluated the sequence, it turned out we’d been missing a portion that was essential for replication. A Japanese group working on the same problem came to the same conclusion at around the same time.
Was that realization enough to clear the way toward finding a treatment?
No. The shifty nature of HCV proved to be another significant hurdle. The replication mechanism of the virus is prone to error. That tendency constantly gives rise to new versions of the virus, enabling it to avoid attacks by the immune system, which may not recognize a particular mutant as an invader. And creating a treatment that works on all versions of the virus was a daunting proposition. How do you know that the genetic target you home in on is exactly the same in all strains of the virus?
Does the diversity of the virus mean that people living with hepatitis C could be housing a virus whose genome differs from the one you were studying in the lab?
Yes, and that was yet another problem we needed to solve. To overcome this issue, we created our own version of the genome, in which each building block of the RNA genome was the one most commonly found in a person infected with the virus. This lab-created version of the virus proved capable of replicating in the liver, just like natural HCV.
This was a critical breakthrough. Using our “consensus” model virus, we were able to show that some viral proteins that people suspected would make good drug targets were indeed essential for HCV to replicate and spread. It was about this time that I moved to The Rockefeller University to establish the Center for the Study of Hepatitis C.
“The story of hepatitis C is really one about persistence. We had to continue believing that success was possible, and continue trying different approaches.”
What was still missing at that point?
Despite its ability to replicate in the liver, our model HCV genome failed to replicate in cell culture. It was incredibly frustrating. We desperately needed a way to study the virus in the lab if we were to make any headway against this devastating illness. The next breakthrough came from taking a consensus HCV genome, chopping out the part that coded for the proteins making the virus particle, and inserting a marker that could be used to select for HCV replicating in cells.
We later found that such HCV “replicons” actually have adaptive mutations that make their propagation in cells more efficient. By making new replicons with these mutations, we were able to provide the first cell-based systems for studying how HCV amplifies its genome inside a host cell. These systems also turned out to be useful for evaluating and discovering new anti-HCV drugs. In the hands of biotech and pharma, they enabled the discovery of drug combinations that can completely eliminate the virus from the body.
But even though HCV replicons could replicate, derivatives that contained the whole HCV genome initially failed to make infectious virus. It was overcoming this last hurdle that got us an efficient cell culture system in which, for the first time, every step in the HCV life cycle could be studied.
Work by many scientists around the world—including Volker Lohmann and Ralf Bartenschlager who first reported on the replicon system—has made this progress possible.
What technological advances were most essential to this success?
Although many technologies contributed, I think the story of HCV is really one about persistence. The most crucial elements were blood, sweat, and tears. We had to continue believing that success was possible, and continue trying different approaches even when we repeatedly encountered failure.
How were you able to sustain such determination?
One standout memory was hearing from a woman whose adopted daughter was infected with HCV. That was nearly 20 years ago. We met and remained in touch over the years. The daughter was treated as a teenager. She’s now married and has a family of her own. When the Lasker Award was announced, I received an email from her thanking me and others in the field. That’s a very rare event for a basic scientist.
We always had in mind the fact that existing treatments were not very good, and people were suffering. Hepatitis C is a global epidemic. Up to 700,000 people were dying each year from liver diseases related to this pathogen. Until we could create something better, patients were limited to treatment with interferon, which often failed and caused harsh side effects.
What discoveries from your HCV work are proving useful in the fight against other infectious diseases?
The methods for determining the missing sequences of the genome, the concept of creating a consensus clone, finding a reliable method for creating a functional replication system for a virus with so much variation—all of these could be useful in other arenas.
Perhaps more relevant, though, is the fundamental importance of supporting scientists in becoming skilled before the need for those skills arises. In my case, my involvement with hepatitis C happened only because of my prior work on yellow fever. No one knows where the next virus threat will emerge or what expertise might be called upon, and no one can predict what research will yield the next biomedical breakthrough. So to enable rapid progress against dangerous new pathogens, we need to continually foster diversity in science.
What is your outlook for the future of HCV?
We actually still have a lot of work to do on this virus, which is why my lab and many others continue to study it. We don’t yet understand much about the pathogenesis mechanisms of HCV infection—how the virus triggers liver scarring or cancer. Although this is becoming increasingly rare, we still need salvage therapies for people for whom the current medications fail.
Ending HCV will also require work beyond the laboratory. Bringing the curative treatment now available to people infected with the virus turns out to be more complicated than we would want. I would like us to do better, nationally and globally, implementing the necessary measures so that anyone infected with the virus can be treated.
How much do these remaining achievements depend on basic science?
A great deal. We all want bench research to lead to new treatments and other meaningful benefits, and I believe any scientist supported by the public good must keep this concern upfront. But it’s also important to recognize that these clinical advances depend on a deep knowledge of fundamental biology. If we don’t support basic science, then a vast world of potential progress will remain unexplored.