Feature
A sugar bomb in disguise
It’s a time-honored, if sometimes ill-advised, tradition in medical research: Try it first on yourself. Thomas Huber’s own weakness for diet soda led to his search for evidence that chemical attempts to fool the human sweet tooth may have unanticipated effects. Now, he is conducting a clinical trial to better understand if artificial sweeteners alter metabolism.
By Wynne ParryAmericans love sugar. We put it in bread, breakfast cereal, yogurt, pasta sauce, salad dressings—all kinds of things that don’t really need it. We invented the waffle cone sundae and the 44-ounce Slurpee. We consume 12 million tons yearly, about 75 pounds per person.
In Europe, the sugar cult is less intense. When Thomas Huber lived in his native Germany, where even the doughnuts are not very sweet, he drank sparkling mineral water every day. But after he moved to the United States, he couldn’t find it as easily. Seeking a bubbly fix, he turned instead to the sappy-sweet, flavored sodas that fill American supermarket aisles. But he was wary of sugar calories, so like many others before him, Huber made a compromise. He turned to diet soda.
It had flavor, it had bubbles, and it didn’t have sugar. Before long, he was working his way through two liters a day.
It wasn’t exactly a healthy choice, Huber knew, but it couldn’t be too bad.
Huber’s move from Germany, where he grew up, happened 16 years ago. And since he switched to diet soda, he’s been consuming aspartame—one of a number of chemicals that beverage makers use in their diet products to take the place of sugar—in large quantities on a daily basis for much of that time.
Huber is a scientist, and it so happens that he studies the receptors on cells that detect things. Things like nutrients, and sweetness. Even so, like the rest of us, for years, he had no reason to doubt that aspartame did exactly what it was supposed to do: trick those receptors into registering sweetness, then pass on through the body without being converted to calories the way sugar is.
But what if things were more complicated than that?
Sugar fuels the body but can be toxic at high concentrations. We crave it—before modern conveniences like cupcake ATMs it signified foods such as fruits and roots, which are nutritious and provided our hunter-gatherer ancestors with quick bursts of energy. But today we eat way too much of it. It causes obesity, hypertension, and diabetes, and public health experts really wish we would cut back.
“The ultimate irony is that aspartame may be contributing to the obesity epidemic, not mitigating it.”
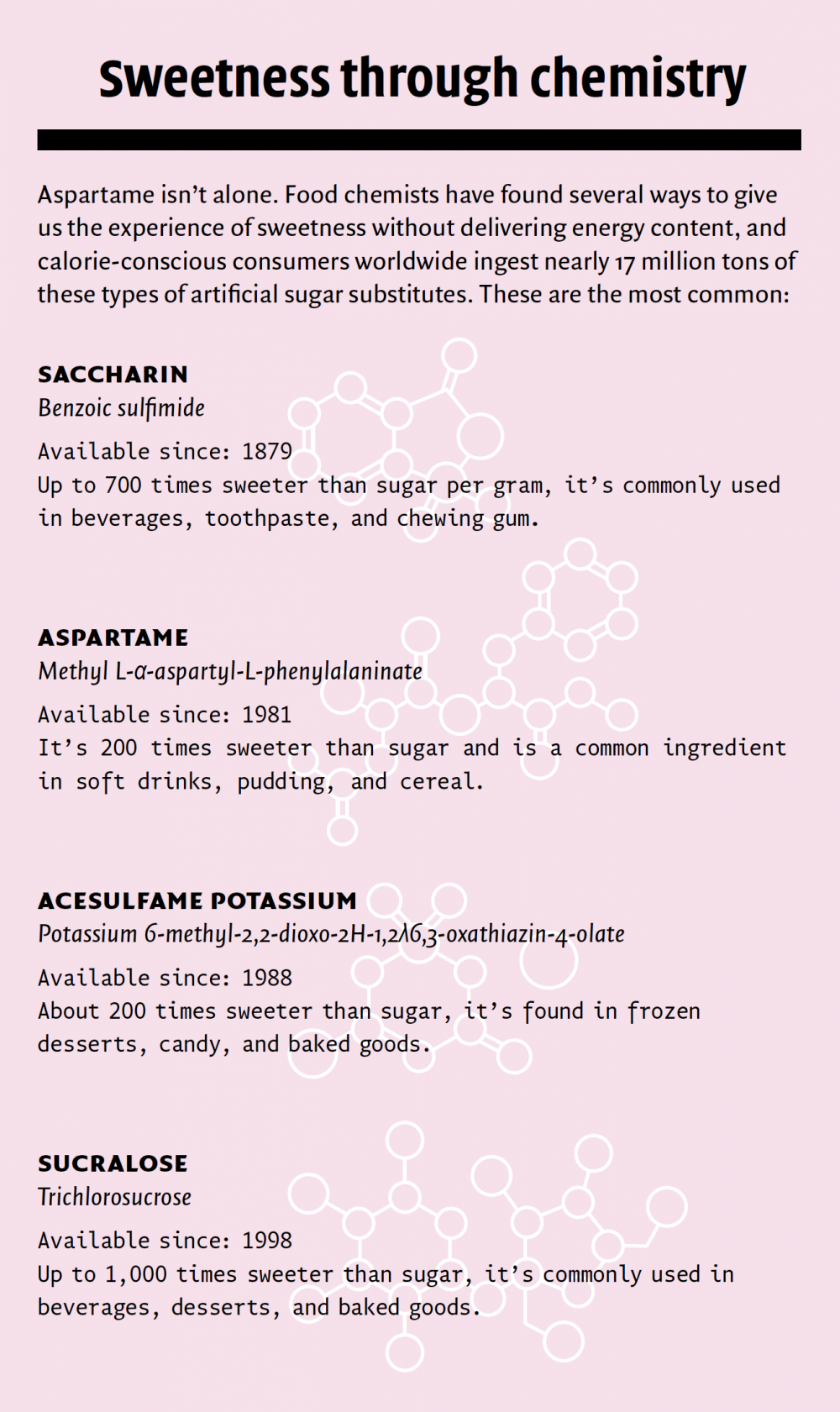
Artificial sweeteners promise better living through chemistry. They have all of the sweetness and, supposedly, none of the consequences. Although a few studies have suggested a link between sweeteners and cancer or neurological problems, the FDA deems aspartame, as well as five other artificial sweeteners, safe. The substances are also cautiously endorsed by medical advocacy groups including the American Heart Association and the American Diabetes Association, who say they can be effective ways to reduce calorie intake and help prevent disease.
There is mounting evidence, however, that artificial sweeteners may have subtle effects on metabolism, the process by which the body breaks down and uses food. In fact, a widely publicized 2014 study in the journal Nature linked artificial sweeteners to disruptions in the body’s ability to control blood sugar, a hallmark of diabetes.
Huber reads Nature. He saw the study, and it made him think of sweetness receptors. It turns out they are not confined to the tongue. Scientists have found them lodged in many organs, including the small intestine, where they help maintain blood sugar at safe levels by detecting the arrival of an energy-rich meal.
“I thought, what if my gut receptors had been activated by artificial sweeteners?” he says. “And, what if by consuming so much artificially sweetened soda on a regular basis, I had overstimulated my metabolic control system, preventing it from responding normally to food?”
Huber had his hypothesis. To test it, he decided to launch a pilot study, on himself. He gave himself an oral glucose tolerance test, typically used to diagnose gestational diabetes in pregnant women. The tools were simple enough: a bottle of water mixed with 75 grams of glucose (the equivalent of 20 sugar cubes) and a $30 blood glucose meter kit from the drugstore.
“Either the results would come back normal and I could happily continue drinking my soda,” Huber figured, “or, if they didn’t, I would stop to benefit my health, and I would have a fascinating project. It was a win-win scenario.”
After fasting overnight, he drank the wince-inducing sugar water and pricked his finger five times over two hours, charting the numbers as his body struggled to control the sugar.
The results were unambiguous. Huber immediately knew the magnitude of this chart’s arc was abnormal. But what he didn’t realize at the time was that his peak blood sugar levels were up by over 30 percent.
He reasoned that if his test results were indeed the result of too much aspartame—if the aspartame had overstimulated the sweetness receptors in his gut—then the effect should be reversible. The lining of the gut renews itself periodically, so over time, the skewed receptors would be replaced with new ones. As long as the new receptors weren’t exposed to aspartame, his metabolism should return to normal.
He moved to phase two of his experiment. For the first time in a decade and a half, he stopped drinking diet soda. He drank sparkling water instead. He avoided anything artificially sweetened, but otherwise ate normally. He went about his business. And three weeks later, he retook the test.
Sure enough, his blood sugar was back to normal.
Huber, a research assistant professor in molecular biologist Thomas P. Sakmar’s lab, showed these observations to his boss, who studies cellular signal transduction. Sakmar, who tends to be fascinated by any finding related even tangentially to his work, was indeed fascinated. A clinical trial was born.
They brought in John Paddock, a Weill Cornell Medicine student who was completing a research rotation in Sakmar’s lab, and with assistance from staff at The Rockefeller University Hospital, they designed and launched a trial using volunteer subjects who already have a diet soda habit.
Molecular biologists like Huber and Sakmar don’t often find themselves running patient studies. “As scientists at Rockefeller, we have the amazing leeway to start with an interesting observation or idea and run with it,” says Sakmar, who is Richard M. and Isabel P. Furlaud Professor. “Even people like us who don’t typically run experiments that involve humans can get the support we need to set up a clinical trial.”
At its outset, the study seeks to link regular consumption of aspartame with problems controlling blood sugar. To this end, the researchers recruit volunteers like Huber—healthy people who drink at least three cans of diet soda a day. Participants take an initial test—an extended version of the glucose tolerance test Huber gave himself—and those showing abnormally elevated numbers are invited back.
This is where it gets interesting. The trial’s second phase investigates whether these abnormalities in blood sugar control can be reversed. For five weeks, the participants move into The Rockefeller University Hospital’s inpatient unit, where they eat and sleep under the supervision of specially trained research nurses. Here, researchers are able to control every calorie and every nutrient they take in. Their meals are prepared in a special kitchen where each ingredient is measured and recorded with precision. Nothing goes into their bodies that Huber, Sakmar, and Paddock don’t know about.
At first, the volunteers continue to drink diet soda. Then, after a few weeks, they stop, and a few weeks later they start again. All the while their precisely controlled diets remain steady, and the research nursing staff document their levels of blood sugar as well as incretins, hormones that help regulate glucose metabolism.
As it happens, incretins are a critical part of this story. They are the keystone in Huber’s hypothesis as well as the subject of much other research on the effects of artificial sweeteners. When activated, intestinal sweet receptors trigger the release of incretin hormones, which in turn prompt the pancreas to release insulin, a hormone that tells cells to take in sugar.
This system helps to ensure good control of blood sugar. Huber suspected that by excessively triggering the gut’s sweetness receptors, artificial sweeteners may be somehow interfering with the incretin response, ultimately leading to problems metabolizing sugar. In other words, the issue may not be with insulin production itself, but with the signaling molecules that turn it on and off.
Others scientists who are not involved in Huber’s study have come to the same hypothesis. Kristina I. Rother, a pediatric endocrinologist at the U.S. National Institute of Diabetes and Digestive and Kidney Diseases, conducts clinical research on the effects of artificial sweeteners, and her work has linked a combination of two artificial sweeteners to increased incretin release when they are consumed before a glucose tolerance test like the one Huber gave himself.
“I am among those who strongly believe that artificial sweeteners do disrupt metabolism; however, until we have long-term studies in human beings, we won’t have proof,” Rother says. “By looking at what happens over the course of weeks, when aspartame is withdrawn from heavy consumers in a controlled environment, Huber’s study has the potential to fill an important gap.”
Meanwhile, experiments by Susan E. Swithers, a professor of psychological sciences at Purdue University, have turned up something quite different from Rother’s work with people. Using rats, she is examining how artificial sweeteners might affect the learned relationship between sweetness and calories, and has noted that after consuming artificial sweeteners, the animals show a decreased incretin response to sugar.
“For a long time, it was assumed that artificial sweeteners were inert; they passed through your gastrointestinal system, and didn’t engage it. We don’t believe that is true any longer,” says Swithers. “Some of us in the field are starting to see that these sweeteners do have consequences. But we really don’t understand what those consequences are or how they come about.”
Firm answers to complicated questions don’t come easily, and running month-long tests on volunteers is slow and expensive. Just finding people who qualify for the study—men and women age 18 to 45 who already have a three-can-a-day diet soda habit—has proved challenging. But Sakmar and Huber believe it’s the best way to settle a question that has enormous public health implications. Aspartame, after all, isn’t found just in soda. It’s in yogurt, chewing gum, ice cream, pudding, breath mints, and all kinds of packaged baked goods.
“The ultimate irony may be that, by interfering with the gut’s ability to properly perceive sweetness, aspartame and other artificial sweeteners may be contributing to the obesity epidemic—not mitigating it,” Huber says. “I suspect the relationship between this unconscious and conscious perception in the brain will be key to fully understanding the effects of these sweeteners.”
Huber himself isn’t waiting for the results. After seeing his blood sugar return to normal on his second test, he gave up his diet soda for good. “I once tried one again, but found it incredibly sweet,” he says. “I am now back where I started: sparkling water, maybe with a splash of fruit juice, if I want to indulge.”