Interview
America is getting vaccinated. Now what?
When the virus struck, researchers responded with unrivaled focus, creativity, and cooperation. Will science maintain its newfound momentum even as this pandemic recedes?
By Eva KieslerFor the past 18 months, the pandemic has wrecked lives, crushed businesses, and tanked national economies. Meanwhile, science has flourished.
In particular, SARS-CoV-2 has become among the best studied pathogens in the history of medicine. And the urgency of the crisis has created focused attention on biomedical research and its importance to our lives, leading to new modes of discovery and launching unprecedented collaborations. The results—vaccines with unmatched efficacy, innovative monoclonal antibody drugs, novel research tools, and more—suggest the possibility of a new normal for science.

How did we get here so quickly, and what challenges lie ahead? Is biomedical research on the cusp of a continuing renaissance, or will the passing of the crisis bring a return of old habits? How will we prepare for the next virus?
We discussed these and other questions with three experts participating in efforts to mitigate COVID.
Theodora Hatziioannou is a research associate professor in the Laboratory of Retrovirology and coauthor of Principles of Virology: Fifth Edition, a leading virology textbook. An expert on HIV, Hatziioannou is now studying how SARS-CoV-2 variants interact with antibodies. She has also played a key role in developing a monoclonal antibody drug against COVID now in clinical trials.

Richard P. Lifton,the Carson Family Professor, is president of The Rockefeller University and head of the Laboratory of Human Genetics and Genomics. As president, Lifton put in place rules and practices that allowed COVID research, and science as a whole, to move forward safely and swiftly at Rockefeller.
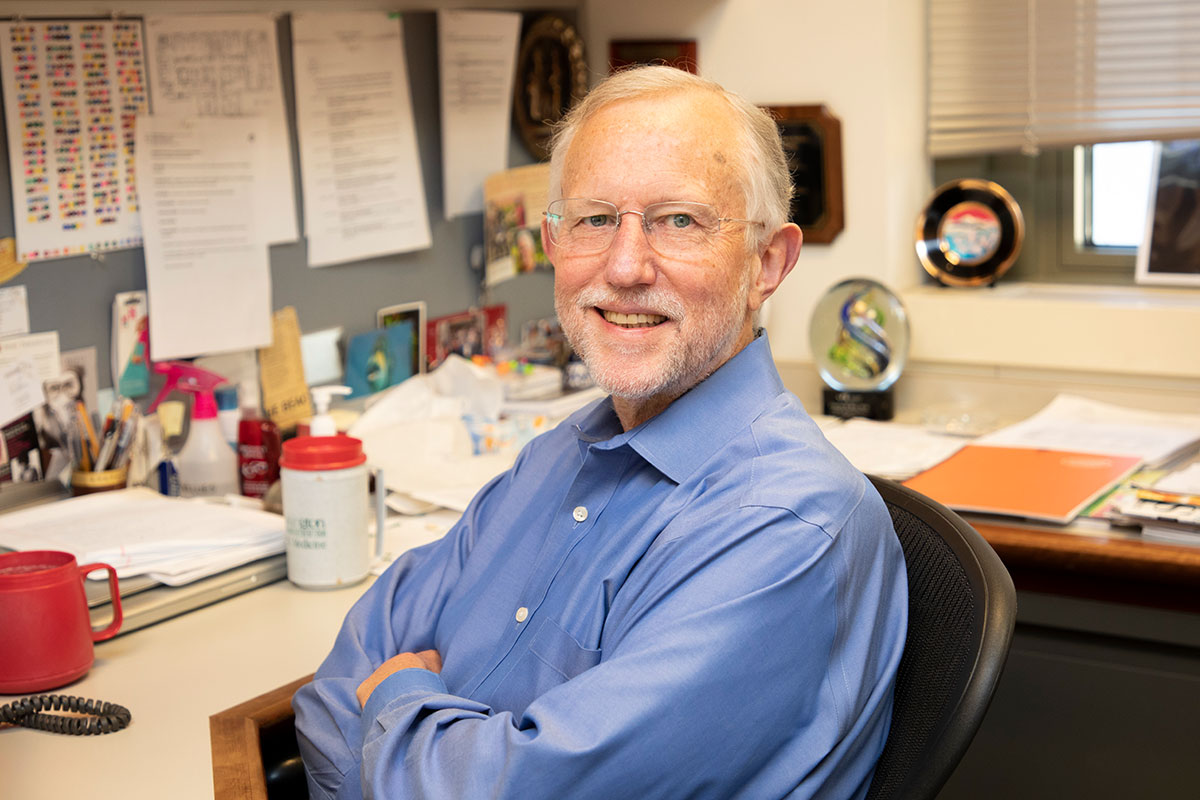
Charles M. Rice is the Maurice R. and Corinne P. Greenberg Professor in Virology and a winner of the 2020 Nobel Prize in Physiology or Medicine. Best known for his work on hepatitis C, which led to a cure, Rice has worked on numerous viral diseases including Zika, dengue, yellow fever, and hepatitis B. Recently his lab identified human proteins that SARS-CoV-2 needs to survive inside host cells, a discovery they hope will translate into new broad-spectrum antiviral drugs.
What has most impressed you about scientists’ response to the pandemic?
TH: The response has been amazing. Here at our institution and across the world, labs began forming tight collaborations, working almost as one, with each person contributing the types of experiments they were good at. The results are remarkable—an outpouring of publications has already impacted how we manage COVID at different levels, from slowing transmission to developing vaccines to treating infected patients. And on a personal level, being part of this movement has been an unforgettable experience.
CMR: I was struck by the sheer number of researchers who stepped up to help mitigate the crisis, many of whom had never before worked in infectious disease. By asking themselves how their expertise could be of help, they were able to come up with creative ideas and approaches. I suspect many of these “converts” will continue to work on coronaviruses or other aspects of COVID-19 after the pandemic is behind us.
Yet it’s important to remember that the many scientific achievements we’ve witnessed over the past year didn’t come out of nowhere. They are the direct result of decades of research aimed at understanding fundamental life processes.
Can you give an example?
RPL: One spectacular example is the development of highly effective mRNA vaccines like Pfizer’s and Moderna’s, which resulted from decades of molecular biology research. Only in recent years have scientists come up with clever ways to use RNA molecules for the development of vaccines and other kinds of therapeutics. They’ve had to overcome significant hurdles, including the fact that the immune system is built to recognize and destroy foreign RNAs when they get into cells.
When the pandemic hit, they had learned how to get around this problem by biochemically modifying RNA molecules. Just in time, the technology was ripe for the opportunity to develop lifesaving COVID vaccines.
CMR: Another thing that turned out to be critical was past research on the SARS-1 and MERS viruses, relatives of the novel coronavirus that also jumped from animals to humans. Historically, very few labs focused on coronaviruses, studying mainly mouse hepatitis coronavirus, but the field was invigorated during the 2003 SARS outbreak and then again with the 2012 MERS outbreak, when there was fear that these highly pathogenic viruses would spread across the globe. These viruses use the spike protein on their surface to gain entry into host cells—which, as we now know, is also the case for SARS-CoV-2.
When the present pandemic hit, scientists didn’t have to begin studying a new pathogen from scratch but could immediately focus on the spike protein, which indeed has turned out to be an excellent target for vaccines as well as for treatments such as monoclonal antibodies. Imagine how much time might have been lost if it weren’t for the early work on mouse hepatitis coronavirus, SARS, and MERS.
With that lesson in mind, do you think the pandemic will cause a lasting shift in scientific priorities? Will more resources be allocated toward virology and infectious disease?
TH: I really hope so. Before COVID, virology was not very well funded. Unless you worked on a major disease-causing virus like HIV, it was very hard to get grants. Now, of course, money is streaming in to support research on SARS-CoV-2.
CMR: Coronavirologists have become the superstars of the day! Whether or not the COVID-19 pandemic experience will lead to sustained funding and changes in public health preparedness remains to be seen.
TH: But it’s hard to tell what will happen once the pandemic is under control. As we saw with SARS and MERS, science policy tends to be rather shortsighted. A new virus emerges, and everyone panics—but once the threat has passed, things have a tendency to go back to how they were.
Maybe this time will be different. There are more viruses on Earth than stars in the universe, so we can’t possibly study them all. But if governments and institutions were to allocate more resources to this field, we’d be able to cast a wider net. This would put us in a better position to respond the next time a coronavirus jumps from bats to humans or some other type of virus shows up in the human population. Because it will happen again, no doubt.
How might we get better at tackling coronaviruses we haven’t yet encountered?
CMR: Among other things, more research into this viral family might allow us to develop an antiviral akin to a broad-spectrum antibiotic—a drug people could safely take if there are outbreaks with viruses similar to SARS-CoV-2. Ideally, one could use such a drug to treat people in the earliest stages of infection to prevent disease and curb further transmission among those who’ve been exposed to the pathogen.
TH: As with interventions against other pathogens, multiple drugs will need to be developed since viruses can acquire resistance to individual compounds. Having multiple drugs also increases the potential for tackling future emergent coronaviruses.
So far the vaccines developed for COVID have been extremely effective. Will they be enough to get us permanently past this pandemic?
CMR: I think vaccines will make a big difference, but we cannot stop there. For one thing, we need to develop treatments and means of prevention for people who can’t get the vaccine because they are immunocompromised, or who choose not to get vaccinated. To that end, there is much promise in modalities such as monoclonal antibodies and small-molecule drugs now being pursued at Rockefeller (read more about this work in Inside the response).
TH: Also, the vaccines being used today will have to be tweaked and further studied going forward. We only began vaccinating people en masse in December, so it’s way too early to know how immunity will evolve after vaccination. For how long do the vaccines work, and how effective will they be against new variants? And how will the virus evolve?
RPL: Beyond answering these scientific questions, there are urgent public health issues we need to address at the societal level. At the beginning of the pandemic, we were totally unprepared to diagnose the disease. We consequently failed to prevent people from getting infected and did not curb the spread of the virus.
Moreover, the pandemic has revealed deep health disparities based on income, race, and ethnicity, underscoring just how broken our public-health system is. This inequity is unacceptable, and we have a long way to go to make sure the vaccines become equally accessible to all citizens. We can do the greatest science in the world, develop the best diagnostic and therapeutic capabilities—but those agents will never have the impact they should if we can’t deliver them to the most vulnerable members of our society.
If national and local governments faltered, the university responded proactively when the pandemic struck. How did this response unfold?
RPL: Our first goal was to keep all members of our community safe while also making sure buildings and facilities remained operational during statewide lockdown. In March of last year, we closed the university while retaining a skeleton staff of about 180 people whose presence on campus was indispensable. From day one, we implemented robust protocols for mask wearing, social distancing, and cleaning, as well as systems for testing and tracing. We had a committee of faculty experts monitoring developments to recommend changes to our practices as we learned more about how the virus works and how it spreads.
Our scientists had no intention of remaining idle. Nearly a third of our labs immediately pivoted to take on projects that would make meaningful scientific contributions to help combat the pandemic. Across campus, an inspiring effort took place to make this possible—reducing the density of scientists in the labs, improving air circulation, and establishing a testing and tracing program to prevent the spread of COVID on campus. We’re fortunate to have a very dedicated workforce that helped keep our facilities secure, facilitated our essential operations, and ensured adequate supplies of PPE and other laboratory supplies we needed to do our work.
Last summer, we began reopening all labs with safety procedures in place, and as this scaled up, we instituted mandatory weekly COVID testing for everyone coming to campus using a robust saliva test developed on campus. With these precautions, we have had no cases of viral transmission on campus throughout the pandemic, testimony to the impact each of us can have by working together to protect one another.

What implications might ongoing COVID research have for other diseases?
TH: The speed and detail at which we are learning how the immune system responds to virus infection and vaccination are just remarkable, and this knowledge is giving us a brand-new tool kit to study immune mechanisms in general. So far, much of what we know about antibody and T-cell responses to pathogens comes from decades of studies mainly of HIV-1, but now we have the opportunity to delve deeper, potentially generating knowledge and technologies that will advance research on virtually any infectious disease. The same is true for vaccines—novel platforms such as mRNA technology will find uses across many diseases in the future.
Also, there is so much we don’t know about how viruses affect the body more broadly. For example, it will be very interesting to figure out the underlying causes of mysterious conditions such as long COVID, or PASC, in which people infected with SARS-CoV-2 may have symptoms for a year or more, and MIS-C, a rare and potentially dangerous side effect of COVID affecting young children. Research in these fields will likely yield knowledge applicable to a host of other post-viral diseases.
During the pandemic, scientists moved quickly to share their results, publishing a deluge of data on preprint servers ahead of peer review. Are cultural changes like this likely to stick?
RPL: The urgency of the pandemic demanded immediate sharing of data and showed that we can move much faster, and conduct investigations at a bigger scale, by working collectively—which we’ve long known but haven’t always been able to operationalize. I’m sure that many collaborations that began in the pandemic will continue and that aspects of rapid dissemination of data via preprint servers will spread through much of the biomedical community. Nonetheless, not all science is advanced by large collaborations, which can get bogged down in bureaucracy and can stifle creativity. We need to be wise in fostering support for the most transformational ideas while selectively applying the advantages of scale when needed.
CMR: Preprint servers have really shown their value during the pandemic. Many researchers are now discussing what role they should play in the post-pandemic era versus how much we should continue to rely on for-profit publishers—especially on boutique journals where the peer review process can take months or years, and the cost of publishing a paper is more than many labs can afford.
I think most scientists would agree that peer review still has a role to play in the academic process, but we need to modernize the systems under which new research and young researchers are being appraised.
What worries you most about the future of the pandemic?
TH: I’m not worried about the science. We’ve seen incredible breakthroughs in a relatively short time, and I think researchers have done everything we could to stay on top of the virus. What worries me more is societal behavior and public health messaging. Simple things that would have helped mitigate the scale of this crisis didn’t happen; measures to contain the spread were relaxed too early.
Vaccination is critical, and it’s still under way. Variants of concern are circulating in the population, and we must keep the numbers down to limit the chance that these variants acquire further mutations that could reverse our progress. There is a way out of the pandemic, but we are not there yet—and many countries in the world aren’t even close. So we need to convince policy makers and the public that, unfortunately, some effort is still required from each and every one of us.