Interview
There’s a reason for those gut feelings
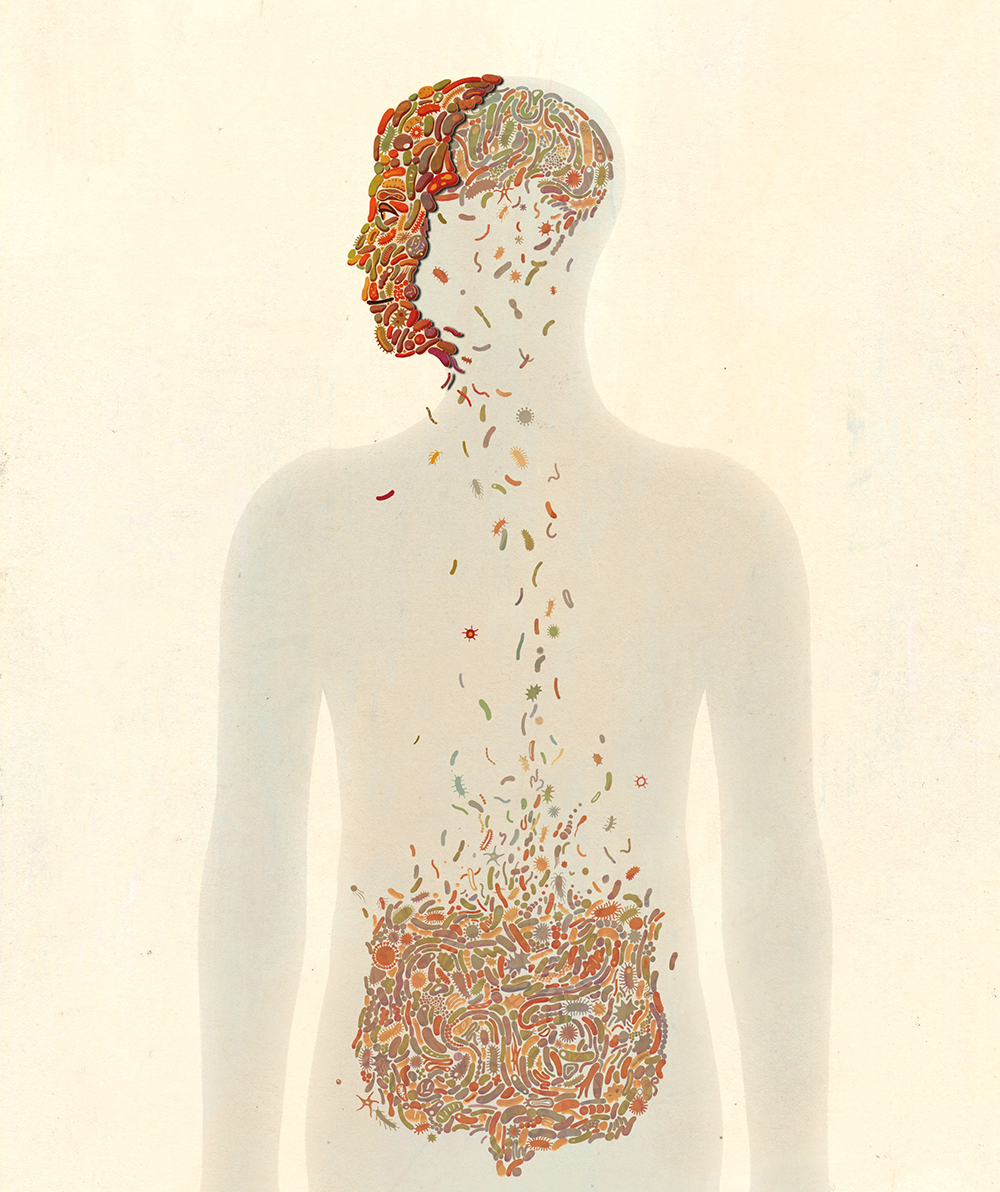
Humans, we are learning, wouldn’t really be human without a little help from the trillions of bacteria we host—many of which interface directly with our own cells. We asked Daniel Mucida about the microbes within.
By Zachary VeilleuxWe tend not to give much credit to the 10 trillion bacteria that line our digestive tracts. Rather, we think of them as docile passengers that, other than perhaps cleaning up scraps of partially digested food, mainly go about their business.
The reality is more complicated. We are as married to our gut microbes as we are to our spouses—with them, in sickness and in health, until death do us part. And as with husbands and wives, our very happiness may well depend on having the right ones.
It turns out that gut bacteria do more than just metabolize our metabolites. They play critical roles in nutrition, weight regulation, and immunity—and there’s growing evidence that their influence goes further. Researchers have found that these organisms directly affect neural activity in the intestines, helping coordinate the processes of digestion and perhaps even affecting behavior, mood, and cognition.
Daniel Mucida, head of the Laboratory of Mucosal Immunology, came to the gut for the immunology—the digestive system is the body’s most active site of immune activity. But he stayed for the neuroscience. It’s hard to study immunity, he says, unless you also account for the activity of cells belonging to other tissues or systems—including neurons, which sense changes in the environment and pass messages between cells.
We spoke to Mucida about the possibility that our resident E. coli are seeping into our thoughts.

What do bacteria living in the intestine and the colon have to do with the neural activity happening far away in the brain?
It’s a common misconception that neural processes occur only in the brain. Yes, the brain is where cognition happens, but every site in the body has neural activity. Unlike most organs, however, the gut has whole nerve cells based in it, not just their extensions. You actually have about as many neurons in your intestine as in your entire spinal cord.
This is why the gut is sometimes referred to as a second brain. It’s able to control complex processes on its own, without input from the brain—including the way food passes through the system, how nutrients are absorbed, and when digestive enzymes are released. The brain is free to focus on other things.
And in many ways, gut neurons—we call them enteric neurons—behave similarly to those in the brain. For instance, it turns out that neurotransmitters such as serotonin and dopamine, which are known to regulate things like mood, emotions, and anxiety, are secreted in the gut as well as in the brain. In fact, about 95 percent of your serotonin is in the gut.
Mood, anxiety—these are things we often talk about feeling in our “gut.”
Yes, they are things that people colloquially ascribe to the gut, and there may be a reason for that. Does the release of serotonin in the gut make you feel something in your gut? At this point we’re not even close to answering this question.
What we do know, based on research in my lab and others, is that there is close coordination between the neurons of the gut and those of the brain. Messages are passed between them. We believe the gut neurons are there to handle the moment-to-moment processing required to maintain digestion, under the broad supervision of the brain.
So how do bacteria fit into this picture?
We are learning that the commensal bacteria of the gut are much more integrated into other physiological systems than previously thought. One of my lab’s interests is to understand how they help protect us from disease, and we have found that healthy, helpful microbes can directly coordinate an immune response. When a bacterial pathogen shows up, they secrete enzymes that stimulate our immune cells.
Similarly, Paul Muller, a recent grad student in the lab, and collaborators, found that our commensal bacteria play an active role in coordinating neurological processes. These bacteria are able to activate a specific neural circuit that connects the gut to the brain. How they do it is not yet clear, but it’s something we’re looking at.
That would give bacteria a lot of power over our neurological processes.
Indeed, we keep finding that bacteria influence the body on many levels. For example, we are intrigued by the prospect that your gut microbiota might affect your appetite and body weight. We have seen in our germ-free animals—mice that are raised in sterile conditions and lack a bacterial environment—that certain neural circuits fail to activate. But when you add microbes to these mice you can activate these circuits and, in some cases, change the animals’ behavior.
For example, we recently showed that gut microbes regulate a circuit that controls blood sugar levels and appetite. When mice don’t have these microbes, their blood glucose levels are reduced; when you add the bacteria back in, glucose levels are restored. We are intrigued by the possibility that the makeup of your gut microbiota could affect your metabolism and eating habits, and maybe also how susceptible you are to pathogens, or diseases, that depend on these dynamic changes in metabolism.
How else can the gut influence behavior?
There are some indications that the gut microbiome plays a role in mood disorders and other psychiatric conditions. For example, we know that some microbes can produce substances that mimic human neurotransmitters like serotonin and bind to the same receptors. These can likely influence mood and behavior, and it’s easy to imagine they might be acting on neurons in people who are prone to anxiety, depression, or neurodegenerative conditions. But, despite some recent advances, this is still an open question.
Likewise, it has been observed that infection during pregnancy increases the chance that the baby will develop an autism-spectrum disorder. And in mice, there is evidence that the makeup of the microbiome of the mother when there is an infection will influence what type of immune-derived molecules—cytokines—develop in the brain of the fetus. These cytokines can influence the development of neurons. In these mouse models, if you change the microbiota of the mother you can actually prevent the development of autism in the offspring.
So how do you change your microbiota?
The most obvious way is through diet. For one thing, the composition of fibers, proteins, fats, and sugars in your meals absolutely does affect what kind of microbes will flourish in your gut. If you change your microbes, you change your metabolism and immune cell composition, leading to altered neuro-immune communications. There are also protein-derived antigens in food that may directly influence the activity of immune cells.
There may be a direct correlation between what you eat and how your neurons behave.
But there’s also a third, very intriguing, possibility. There may be components of the diet that can be directly sensed by the gut nervous system. This would imply a direct correlation between what you eat and how your neurons behave. Some of these relationships are known—capsaicin, for example, the active component of chili peppers, binds to the cation channel TRPV1—but the role of nutrition is understudied in both neuroscience and immunology. In the interface between the two fields, a lot of interesting questions remain unexplored, such as how dietary components that trigger food allergy in susceptible people can interfere with neuronal activity and animal behavior.
What happens when important gut bacteria die?
Normally, the gut is able to maintain a balanced system. There is likely some mechanism in place to keep certain species in check. But you can see how there might be a connection between dysfunction in the body and diseases we think of as infectious in nature, such as C. difficile. And it’s worth mentioning that some of these diseases disproportionally affect people with psychological disorders and mental illness. It’s dangerous to assert directionality here—what’s causing what?—but that’s something we hope can be better defined as the field matures.
How do we get to these answers?
The field is still very much in its infancy, but I think it’s important to ask questions about the human body as a whole. Separating biology into fields such as microbiology, immunology, and neuroscience will only get us so far given how closely interrelated these systems are. Immunologists can no longer study the immune system in isolation; immune cells are influenced by everything else that is happening in and on the tissue, including the complex society of microorganisms residing there.
And it’s a great time to be an immunologist. Because we have collaborations with neuroscientists, microbiologists, cancer biologists, and others, my lab has been able to go in many surprising directions.