
Feature
Lab Partners
By Bethany BrookshireAt 18, Willow Pickard was an open-hearted, artistic soul.
She loved drawing and painting, and jam bands like Phish. The slender girl in a tie-dyed t-shirt—with a mop of curls just like her mother’s—befriended everyone, especially those who needed it most. “The word ‘protective’ comes to mind,” says Julie Newcomb, Willow’s mother, a medical coding analyst based in Livonia, New York. “People that would get bullied or picked on, or people that are a little bit different…she would sort of put her wing around them.”

For years, Willow had been plagued by strange symptoms. Abdominal bloating, strange feelings of fullness, stomach discomfort. “The symptoms were so vague, that’s part of the problem,” Newcomb says. Blood work showed nothing, the doctors could feel nothing. Clinicians blamed hormones or anxiety. “Who the heck isn’t anxious in this day and age?”
The symptoms persisted, but doctors followed protocol and nobody suggested imaging. By the time there was imaging, Willow was 18 and had just started her first year at a community college in Rochester, New York. She had a boyfriend and had started art classes. Now, she also had a diagnosis: Stage IV fibrolamellar hepatocellular carcinoma, sometimes shortened to “FLC,” or just “fibrolamellar.”
Fibrolamellar is not like most other cancers. It is incredibly rare, diagnosed in one out of every five million people. It is a liver cancer that erupts in people who are seemingly healthy. They are also young—most patients are between 11 and 25. In the United States, only a few hundred people are living with it. By the time of Willow’s diagnosis, she already had FLC tumors elsewhere in her body.
Doctors tried multiple surgeries. They tried chemotherapy. Willow got a part-time job at a juice bar and began thinking deeply about wellness. “She was on the computer a lot, researching her diagnosis and some treatment options,” Newcomb says. In the process, she came across the work of Sanford M. “Sandy” Simon, a cellular biologist and biophysicist at Rockefeller. Simon’s lab has focused on FLC since 2009. But it isn’t just the focus on such a rare disease that distinguishes his lab. It also operates in a unique way: Simon makes a point of welcoming FLC patients into his lab, whether they want to just visit or pick up a pipette themselves.
Ten years ago, this cancer was a black box. The past decade has seen a stunning run of discoveries.
Willow visited the lab, participated briefly in research, and donated blood and tissue from her surgeries to Simon’s work. She passed away in 2018 at the age of 21. But meeting patients like Willow “makes you realize your research isn’t just a job,” says Mahsa Shirani, a postdoctoral researcher in the lab. “You want to do something important, because you see the application.” The sense of urgency, she says, is palpable.
In turn, the lab’s distinctive approach to research collaborations has resulted in a stunning run of discoveries—leading to new avenues for treatment and clinical trials. When Simon began his research into fibrolamellar, the disease was a black box. Ten years later, his team has already found the specific mutation that causes the cancer and has identified promising drug candidates to shrink tumors and attack the mutated molecule that causes it. Moreover, they are finding that their deep study of one rare cancer is generating insights that could advance understanding and treatments for others.
Dogged Pursuit of Knowledge
Before 2009, Simon’s Laboratory of Cellular Biophysics had been focused on basic cell biology. With training in cell biology and biophysics, Simon, who is Rockefeller’s Günter Blobel Professor, was interested in how proteins in a cell move from one location to another. He also was curious about how viruses assemble, studying diseases such as HIV and Ebola.
All that changed when his daughter Elana was diagnosed with FLC in 2008. The cancer had no recommended therapies. It was rare—any university or hospital had only a few cases and little information about them. One of the few published studies had survival at five years close to zero.
After the removal of her FLC mass in 2008, Elana has remained cancer-free. But Simon found himself dismayed by just how little was known about FLC. He began to pivot the focus of his lab—starting with Elana, who worked in the lab through high school—and helped discover a DNA mutation common to every studied case of FLC. Simon’s team never looked back.
“I think [Simon] really made the major contribution to the understanding of the disease in the last 20 years,” says Michael LaQuaglia, a pediatric surgical oncologist and collaborator of Simon’s at Memorial Sloan Kettering Cancer Center.
The DNA mutation that Elana helped reveal is one of several breakthroughs. It’s a joining of two genes. The genes usually lie next to each other. The first, DNAJB1, contains the code for part of a heat-shock protein that responds to cell stress. The second codes for part of the enzyme protein kinase A—a critically important protein that helps control the actions of other proteins in the cell.
In FLC tumor cells, however, the genes don’t lie next to each other. The gap between them has been deleted, and the two get transcribed and translated into a protein conglomeration—a chimera. The lab has since shown that the mutation is spontaneous, not something that can be inherited.
This sudden cellular chimera can kickstart tumors. So one angle Simon’s lab is pursuing is to attack the rogue protein itself using something called a PROTAC—a proteolysis targeting chimera, or molecule that will grab the rogue proteins and label them as cellular trash. Another method is using specialized RNAs to silence the RNA that makes the bad protein.
Both of those research pathways have been successful, but Simon wanted something faster—an already approved drug that doctors could add to their toolkit now, instead of waiting years for clinical trials and approval. Instead of assuming their own scientific genius would find a new compound, he says, why not “just screen every drug that’s ever been safety tested for any condition?” The lab went on to screen roughly 7,000 drugs—and found a few that shrank FLC tumors. A combination of one of those drugs and one PROTAC is currently moving toward a clinical trial.
Patients and Persistence
Rare cancers are especially hard to study; with few patients, there’s little information, and very few samples are available to learn more. That was, in part, why Simon and his wife, Rachael Migler, started the Fibroregistry. The patient-community-based group’s goal is to bring science to the patients, and the patients to the scientists. If specific institutions didn’t want to share their data, patients could do it on their own. Information on their history and outcomes could be shared across institutions and even countries. Since it was being run by the patient community, the registry could stay in touch with patients long after they left the hospital or finished a clinical trial. Currently, about 250 patients have completed the questionnaire to join the registry. It’s not a light lift. “There are several hundred questions,” Migler says. The questions can seem utterly random, each trying to pull out any tiny piece of information that might be valuable. Was the patient bitten by an animal at any point? Was it a squirrel? A monkey? Does the patient have pierced ears? Wounds on their feet? “It is basically our attempt to find the needle in the haystack.”
The results have been invaluable for both patients and clinicians. Now, scientists and patients have learned that if caught early enough, tumors can be taken out with surgery, or a patient may receive a liver transplant. These patients have a 44 to 68 percent chance of surviving for another five years. However, if surgery isn’t an option, or if the tumors have spread to too many other parts of the body, survival after five years drops to two to 17 percent. And while chemotherapy can help in other cancers, the registry has shown that for FLC, most chemotherapy has no effect or actually reduces chances of survival.
The registry, doctors, Facebook groups, and internet searches all lead patients to Simon’s lab. He receives four to five emails per week from patients and their families. He replies to each, answering questions, sharing papers, and offering what comfort he can. In turn, contributions of information to the Fibroregistry—whether information or patient tissue—have resulted in four research publications on the disease. The studies explore topics ranging from which patients have better odds of survival, to creating organoids from patient cells to better study the cancer, to the clinical outcomes of treatments like immune inhibitors.
The lab is always looking for new angles on the disease. Jeannie Carreiro, a first-year bioscience graduate student in Simon’s lab, is hoping to use gene-editing techniques like CRISPR to determine what, exactly, allows FLC tumor cells to thrive. But any knowledge she obtains, she notes, is worth it: “We know from our past successes that any detail matters; any detail can help.”
These details could be critical to more than FLC. For instance, tumor-suppressor genes were originally found in retinoblastoma, a cancer just as rare as FLC. Mutations in those tumor-suppressor genes are now known to play important roles in breast cancer, colorectal cancer, prostate cancer, and more. The enzyme isocitrate dehydrogenase plays an important role in cell metabolism. Mutated forms of it were identified in a rare glioblastoma, but they have now been found in other cancers such as acute myeloid leukemia. By digging deep into FLC, Simon hopes that some of the findings could translate to other cancers—both rare and common. As part of that, his team has formed an international consortium of scientists, working together as part of the Cancer Grand Challenges program. The goal is to apply the Simon lab’s approach of making PROTACs, or degraders, to other cancers, such as Ewing sarcoma, rhabdomyosarcoma, and neuroblastoma.
Simon hopes some of the findings could translate to other cancers, both rare and common.
Sometimes, patients coming to visit the lab end up staying to work—weighing in on projects and conducting research, as their treatment schedules permit. Simon tries to treat them like every other lab member, while accommodating some of their medical needs—many of which are side effects of the chemotherapy drugs or surgical recovery.
That includes making sure patients get a full New York City experience. During one of Willow’s visits, for example, Simon found out that the band Phish would be performing in Madison Square Garden. Because of her treatments at the time, however, a regular ticket would have been impossible for Willow. She had to be within 10 feet of a bathroom.
Simon, who used to play in a band, realized his old connections could be of use. “I said to my friends, ‘Listen…I know there are these corporate suites, where they’ve got their own bathroom in them,’” he says. “‘Do you know anybody who can get me two of those tickets?’”
He found a suite; Willow got her Phish show.
A Rare Cancer, A Rare Lab
Simon’s spacious, airy lab is right on the water and has stunning views of the East River from every desk. But lab members don’t spend much time staring out the window. They are planning experiments, conducting research, and analyzing data. Occasionally, when a new patient’s donated tissue comes in from a surgery, the lab is all hands on deck, processing precious samples as fast as possible. Shirani has, like other lab members, on occasion, curled up for a refresher nap in the dark, quiet patient records room. Like all members of the lab, she knows that fibrolamellar patients are relying on her. Not on scientists in general, but on them specifically.
Every patient that passes through the doors of the Simon lab affects the researchers there.
Shirani came to Simon’s lab after doing her graduate work with Barbara Lyons, a chemist at New Mexico State University in Las Cruces. Lyons’s lab had focused on breast cancer. In 2015, her son, Jackson Clark, then 20, was diagnosed with FLC. A devoted chemist like his mother, Jackson went on to pursue a master’s degree in chemistry at Cornell University in Ithaca, New York, in between his surgeries and treatments. He also spent a summer in Simon’s lab, working on the chimeric protein that causes the disease. His work contributed to a 2023 paper showing that fibrolamellar tumor cells behave differently compared to normal liver cells—they produce much larger amounts of ammonia. FLC patients frequently die from the effects of ammonia buildup in the brain; the paper explains why conventional therapies have not worked, and what might. Jackson’s lab work could one day help prevent these deaths.
Jackson passed away in 2020. His mother, Shirani, and Simon are still publishing together, investigating how the fusion gene so key to FLC leads to tumor development, and identifying new immunological targets for potential treatment.
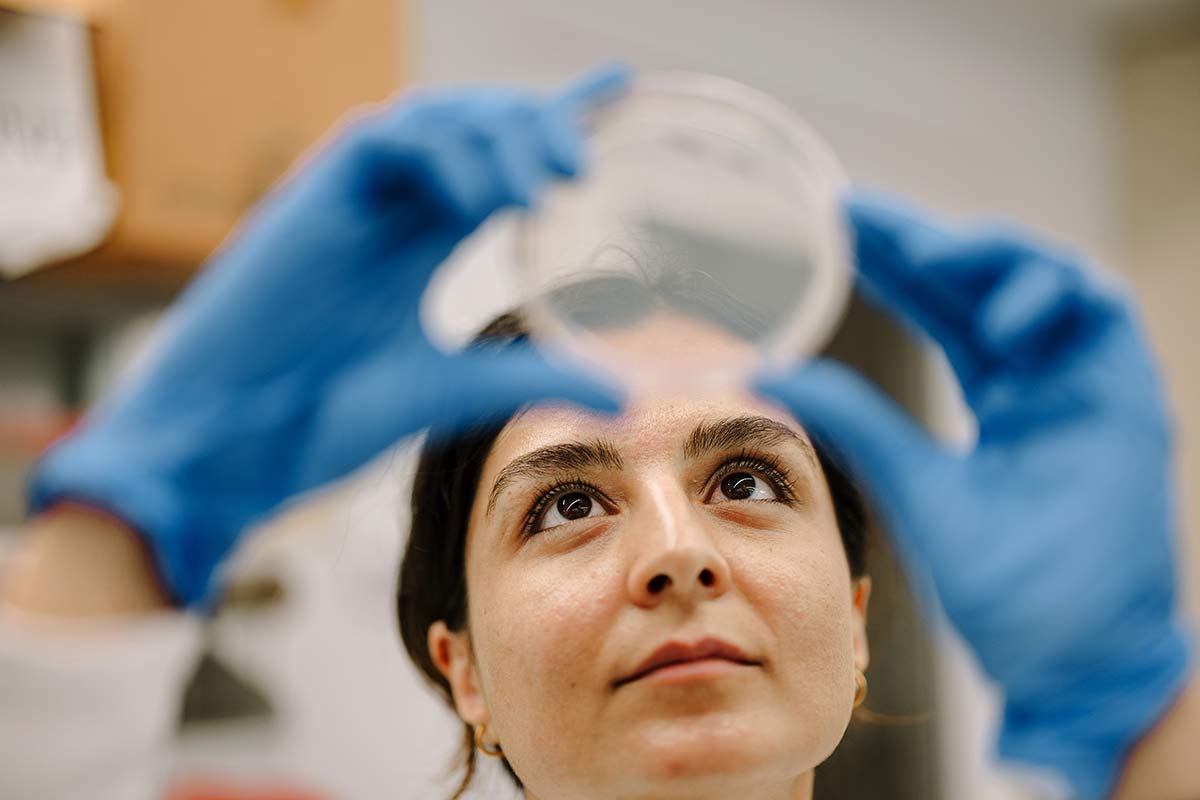


Like Willow, Jackson contributed tissue, blood, and more to Simon’s efforts. Shirani knew him well, and one day she found herself working with his cells. “I remember I was imaging Jackson’s sample at some point,” she says. “And [Lyons] was in the lab. And we were just looking at the picture.” She wanted to tell Lyons that they were Jackson’s cells. She could not make the words come out.
The presence of patients also encourages lab members to work together, not in competition with each other. Lab culture at some institutions can get very competitive, says Jaelyn Vigee, a first-year graduate student in cancer immunology. “We don’t have that. I feel like we’re all just very much trying to work together,” she says.
Michael Ortiz, a pediatric hematologist-oncologist and collaborator of Simon’s at Sloan Kettering, sees other ways such a close connection to the project impacts the science. For instance, calling a new drug the “most effective treatment yet” for treating a cancer might not be wrong. But it might also leave patients with false hope of a cure. The new drug might stop the cancer from growing, or slow it for a while, and then it might grow again. Saying it that way “is less exciting, but is more honest and comprehensive,” Ortiz notes. “My impression is that having someone in the lab with that very cancer helps to ensure more nuanced kinds of claims are made.”
But the success of these collaborations is attributable to Simon himself, a person who is driven, but also kind, say colleagues. “Sandy is unique,” notes Lyons.
Newcomb would agree. Willow has been gone for seven years now, but Newcomb still receives notes from Simon when he publishes new studies on FLC. “It gives me chills,” she says, “because she’s part of these findings.”