Feature
Cancer’s big appetite
All living things must eat, and cancer cells are no exception. A fresh look at cellular nutrition is yielding new ideas for shrinking tumors.
By David NoonanThere’s no shortage of ways to kill a cancer cell. Cut it out, poison it, blast it with radiation, shower it with killer immune cells—they all get the job done. But there is a shortage of good ways to kill cancer cells. One that knocks out all the bad cells in one swipe, leaving the good ones unscathed, and that doesn’t allow the disease to return. We have yet to find that perfect treatment, whether it’s one miracle drug or several therapies cleverly combined. Until we do, cancer will continue to kill, and the medicine that stops it will continue to hurt.
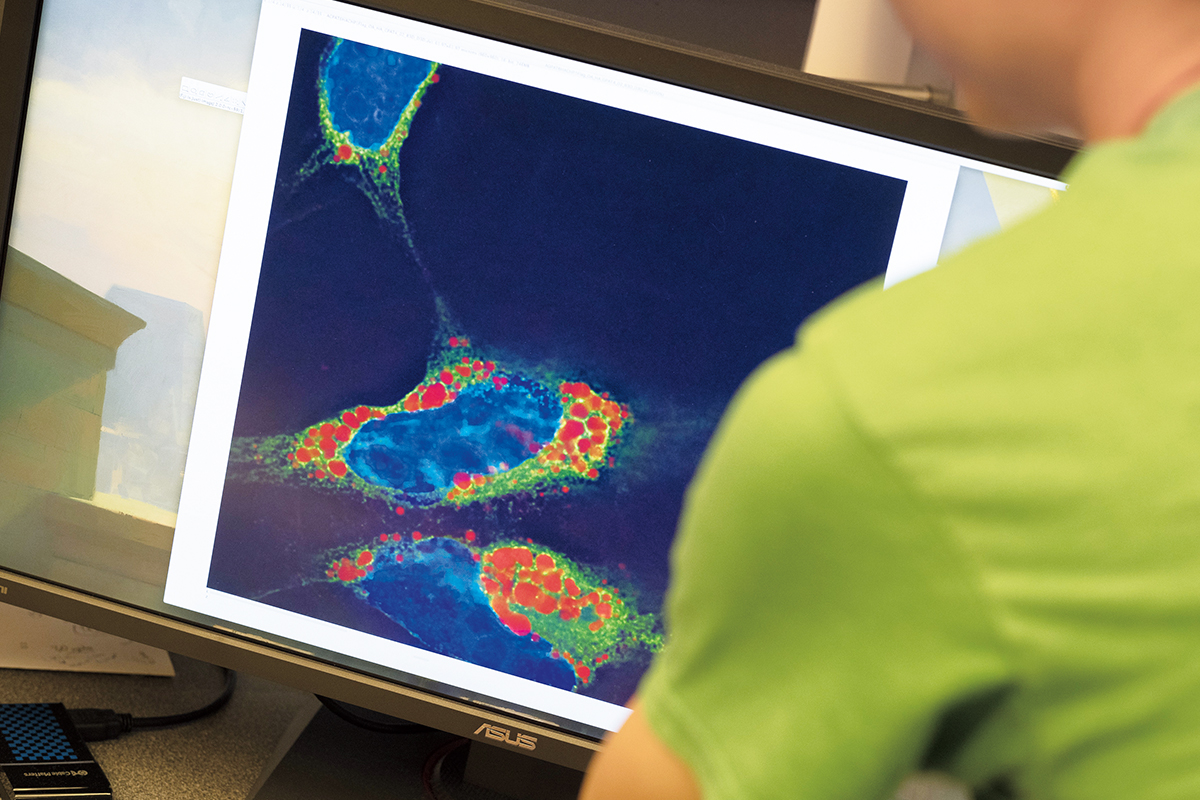
For Kivanç Birsoy, the ideal cancer treatment doesn’t kill cancer cells with violent attacks at all. He wants to simply stop feeding them and let them die.

Birsoy, the Chapman Perelman Assistant Professor, has taken this simple premise—that cancer cells need nutrients to survive—and built a sophisticated research program around it. His work is driven by a vision of the future where patients survive as their tumors, starved of the nutrients they depend on to grow, wither away. The key to defeating cancer cells, he says, is to understand their metabolism.
Like many good ideas, Birsoy’s is not new. The study of cellular metabolism began almost a century ago and has long been perceived as settled science. The textbooks have been written, the Nobels awarded, and the world has moved on to sexier subjects.
First we figure out what cancer cells need that other cells don’t. Then we devise a way to deprive them of it.
But the scientists who pioneered the field, who asked the important questions and wrote those textbooks, were limited by their experimental tools, Birsoy explains as he sits in his office in Rockefeller’s newest research building. “With the tools we have now, genetic tools, I can go back and ask those questions again,” he says, “and get more sophisticated answers.”
When it comes to metabolism, cancer cells are remarkably adaptable. They have several tricks they can employ to maintain their growth, even in the face of inhospitable conditions that would leave other cells lifeless.
For one, they can tweak their own metabolic processes, a lethal power that is unique in human biology—heart cells can’t do it, brain cells can’t do it. Deprived of sufficient blood flow due to a heart attack or stroke, those normal tissues die. But cancer cells are somehow able to hunker down and pull through, and, having survived these hostile conditions, they go on to thrive and multiply.
Still, there are some nutrients even cancer cells can’t live without, which is why they have a second trick up their sleeve: the ability to import what they need from the environment instead of producing it themselves. And it is here that Birsoy sees an opportunity. Working with cells derived from lung, breast, blood, and other types of cancer, his plan is to figure out what cancer cells need that other cells don’t, and then devise a way to deprive them of it.
Cancer cells grow fast. In fact, their ability to grow and divide rapidly, and outpace the cells of healthy tissue, is exactly what makes them so deadly. But fast can mean sloppy. Although cancerous tissue can create its own blood vessels, for instance, the new supply is often not enough to meet the cells’ demand. Despite their varied diet, they find themselves facing a scarcity of the oxygen and nutrients they need to survive.
In an experiment, Birsoy subjected 28 cancer cells lines derived from patients to low oxygen conditions. None of them were able to synthesize an amino acid called aspartate, which they require to grow. But six of the 28 overcame this hindrance by altering their metabolism and ingesting aspartate from their surroundings. And having successfully outsourced aspartate production to their neighbors, these cells continued to grow, divide, and proliferate. Like most of Birsoy’s work, the study was done in vivo, using tumor tissue grafted onto mice, a method that provides a more complete picture of biological events than experiments conducted in cell culture.
The findings excite Birsoy for two reasons. First, they provide clear-cut evidence supporting the general hypothesis that cancer cells are able to alter their metabolism to get the nutrients they need to grow. And second, they show the importance of aspartate in particular; tumors can’t grow in low oxygen settings without aspartate, which makes limiting its availability a potentially viable cancer therapy.
Such a treatment, he believes, would target cancer cells without affecting nearby healthy tissue.
Sixty-six years ago, a series of studies began that led to a similar discovery. Researchers working with guinea pig serum found that cells with a particular form of cancer, acute lymphoblastic leukemia, are unable to produce an amino acid called asparagine. It’s similar to the situation with aspartate, with a key difference: The inability to produce asparagine was due to a rare internal anomaly, not an external factor like oxygen level.
“There is a small fraction of cancers that cannot make certain metabolites or nutrients that all other cells are able to make,” Birsoy explains. “So they naturally become dependent on taking it from the outside.” Since the 1960s, oncologists have exploited the leukemia cells’ asparagine dependency by treating patients with a drug called L-asparaginase, which depletes all the asparagine in their blood. As a result, the survival rate for acute lymphoblastic leukemia, which typically strikes children between ages two and 10, has reached nearly 90 percent.
Birsoy wondered whether there were other blood cancers with the same kind of rare defect—cells that were unable to make necessary nutrients and that could therefore be targeted by depleting that nutrient. Soon, his group found a rare cancer called ALK+ anaplastic large-cell lymphoma whose cells can’t synthesize cholesterol, an essential building block for membranes. “If you deplete cholesterol from the environment,” says Birsoy, “these cells die, even though normal cells don’t care.” It was the first such discovery since 1953.
With the advantage of tools that earlier researchers could not have imagined, including a CRISPR-based genetic screen that targeted 200 enzymes involved in the metabolism of the ALK+ lymphoma cells, Birsoy quickly honed in on the culprit. (Among other things, CRISPR, a gene-editing system, makes it possible to deactivate a specific gene in a cell in order to determine what the gene does and whether the cell can survive without it.)
In this case, when the gene for a specific receptor, LDLR, was knocked out by the CRISPR screen, the cells died because they could not import cholesterol from the extracellular environment. That makes the LDLR pathway what Birsoy calls a targetable liability, one that could be exploited by devising a treatment to prevent the lymphoma cells from taking up cholesterol.
The decades-long gap between the asparagine and cholesterol discoveries, Birsoy says, wasn’t for a lack of trying. Postwar scientists in fact spent a great deal of effort hunting for additional metabolic dependencies, but they were held back by the limitations of their methods and technology. Then, in the 1980s, the search for cancer genes took center stage and fundamental metabolism research went out of style.
“Because these pathways were in biochemistry textbooks, there was supposedly nothing left to learn about them.”
“I think people thought they knew everything about it and that it’s boring,” Birsoy says. “Because these pathways were in biochemistry textbooks, there was supposedly nothing left to learn about them.”
Now, cellular metabolism is attracting a new generation of scientists who are using 21st-century tools to revivify the field. Birsoy, a native of Turkey, is a Rockefeller alumnus who did his graduate work in Jeffrey M. Friedman’s lab, where his focus was obesity. As a postdoc at the Whitehead Institute, his interest shifted to cancer. In order to study the metabolism of tumor cells, he began to design new tools, including an instrument for mimicking the nutrient-deprived environment within tumors.
There are many good reasons to learn more about cellular metabolism. For Birsoy, a major one is finding new ways to curb cancer, but he has other applications in mind as well. Every cell in the body converts nutrients into energy, and the recipes they use are diverse. If Birsoy’s work can uncover new details into the workings of, say, fat cells or pancreatic cells, it could lead to a new framework for understanding obesity or diabetes.
Of particular interest to Birsoy are mitochondrial disorders. When he talks about them, you can hear the mix of fascination, frustration, and resolve that drives so much of his work.
“With mitochondrial disorders,” he says, “as with other inborn errors, we know what the problem is, we know the genetics. But we don’t know how to connect the two.”
In some cases, mitochondrial disease makes people deaf; in others it causes seizures; and in still others the result is neuropathy or muscular atrophy. And despite decades of research, Birsoy says, scientists still have no clue why dysfunctions of mitochondria, the cellular organelles that process nutrients into energy, cause these disorders. All we know is that somehow a metabolic process has gone awry.
Birsoy’s work has shown that mitochondria play an important role in synthesizing aspartate, the same amino acid that cancer cells sometimes steal from their neighbors. When those mitochondria are dysfunctional, he says, their aspartate levels are low—and supplying the cells with aspartate restores their function. Birsoy suspects that aspartate depletion might be a root cause of the mitochondrial disease, and that supplementing aspartate might be an effective treatment strategy. But it’s a theory that remains to be tested.
As with cellular metabolism, our understanding of how mitochondria function got frozen at some point in the history of biological discovery, Birsoy says, and it hasn’t been revisited. In some sense, we don’t even know what mitochondria are. The initial idea was that they were a powerhouse organelle, but that’s clearly not the full picture, and they probably do different things in different types of cells. “It’s time to go back and figure out exactly what the function of mitochondria is in different cell types,” Birsoy says. “In neurons, what’s the function? In muscle, what’s the function? And in cancer cells, what’s the function?”
Metabolism is universal—every cell needs nutrients to survive. And although Birsoy’s work has enormous potential, there’s also a mountain of his predecessors’ aging experiments to revisit.
“The way I look at this is, if you don’t have a cure for something, that means you don’t know enough about it,” he says. “We treat cancer and people may live five weeks, five months, or five years longer with existing therapies. But too often the treatment fails and the patients die. And that means there is a lot more to discover.”
Regardless of what the textbooks say.